Nicola Thomas
RN, BSc (Hons), MA. PhD
Professor of Kidney Care
London South Bank University, UK
nicola.thomas@lsbu.ac.uk
2.0 The History of Haemodialysis
Learning Outcomes
- To understand how haemodialysis began
- To identify the challenges that doctors and nurses had to overcome in developing haemodialysis as a therapy
- To appreciate the patient perspective and experiences of home dialysis in the 1960's and 1970's
Introduction
The introduction of Haemodialysis (HD) as a life-saving treatment for end-stage kidney disease was not the result of any large-scale research programme, but rather it emerged from the activities of a several pioneering individuals in the USA and later across Europe.
2.1 The beginning of Haemodialysis
Although HD as an accepted treatment for renal failure was not initiated until the 1960’s, there had been developments in the previous 100 years. The first time that the term ‘dialysis’ was used was in 1854 by Thomas Graham, a Scottish chemist1. In 1913, the first paper on the technique of HD, including the concept of the ‘artificial kidney’, was reported. At this time, experimental dialysis was performed on animals, by using a variety of compositions of dialysis fluid2. The first dialysis treatment performed on a human was carried out by the German physician, Georg Haas, in Giessen, Germany, in the latter half of the 1920’s. He performed six treatments in six patients, but unfortunately, he was not supported by either his hospital or his colleagues, so by the late 1920s the work was stopped.
In 1923, Heinrich Necheles experimented with layering of membranes, thus giving an increased surface area without the necessity for multiple dialysers. The membrane that was used was a sheep peritoneum. Because the membrane was prone to expansion, support sheets were placed between the layers of membrane, thus allowing a large surface area of membrane to come into contact with dialysis fluid. The 1920’s and 1930’s saw great advances in synthetic polymer chemistry, resulting in the availability of cellulose acetate which could be used as a membrane for dialysis treatments. William Thalhimer, used cellophane, a form of cellulose acetate, as a potential dialysis membrane3.
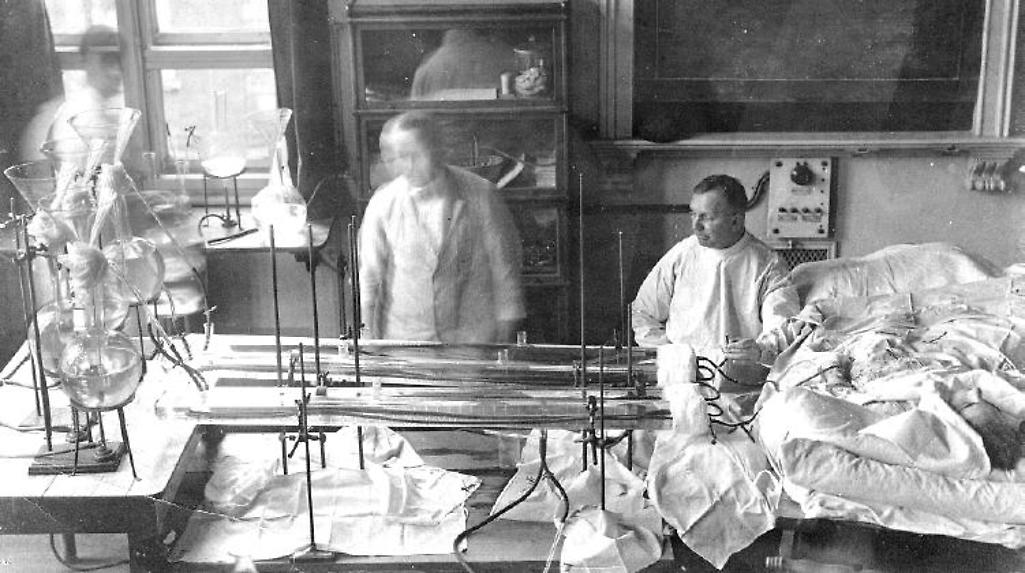
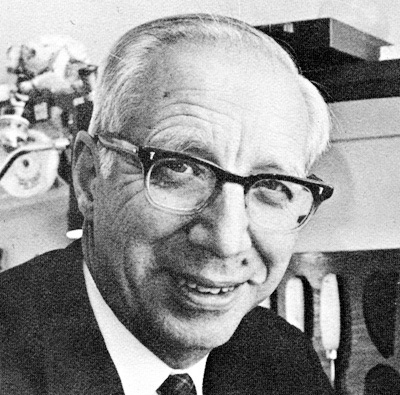
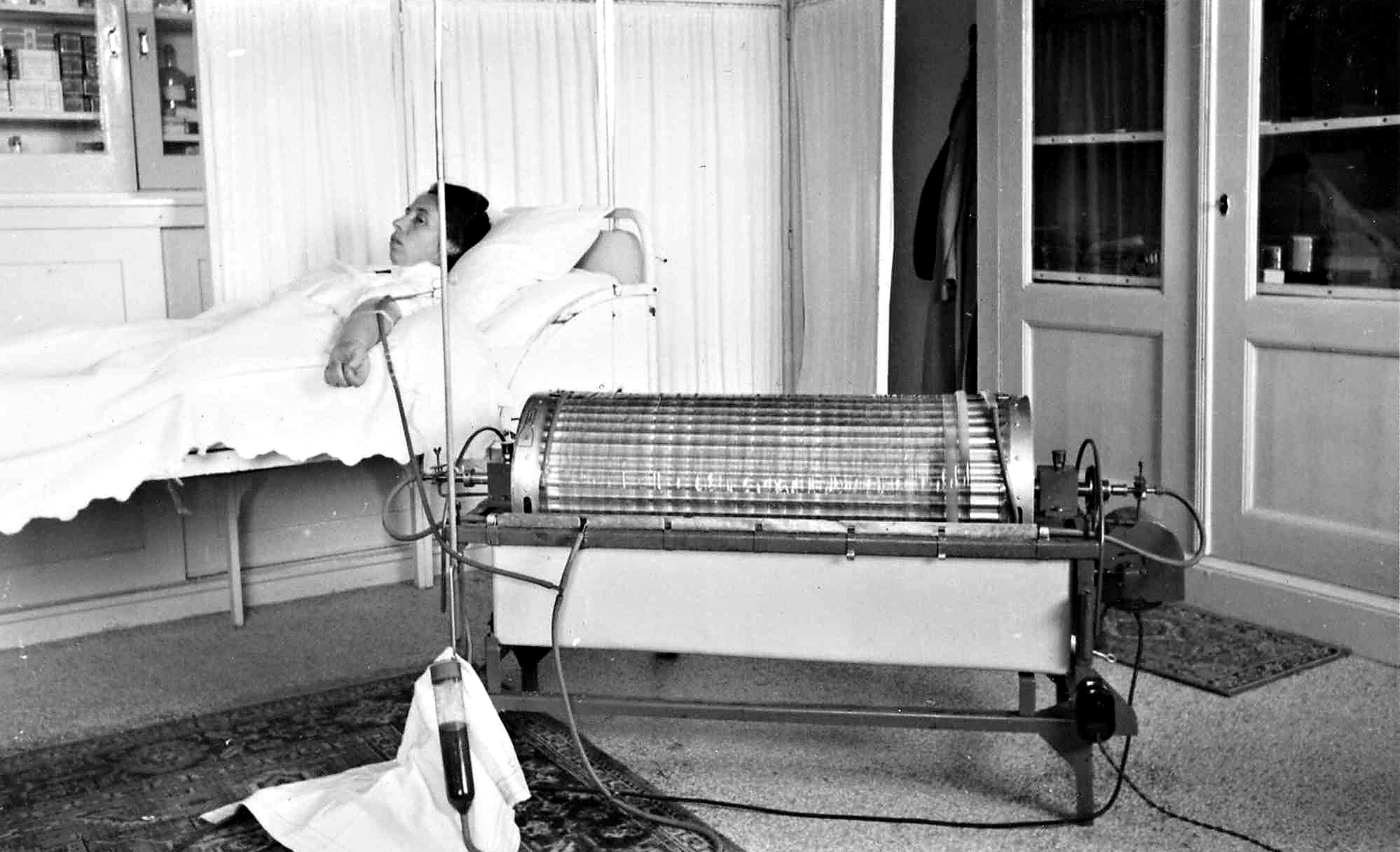
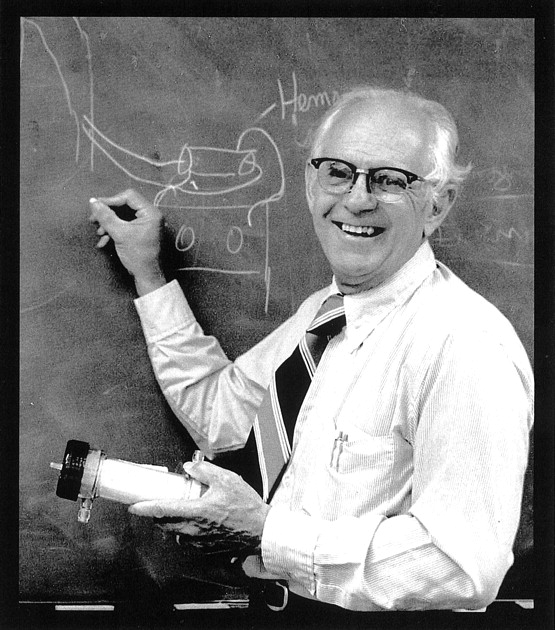
Willem Kolff, became aware of the work of a colleague who was concentrating plasma by using cellulose acetate as a membrane immersed in a weak solution of sugar. He built a rotating drum dialyser which provided sufficient surface area for his first attempt at human dialysis4. His machine consisted of 30 meters of cellophane tube that was wound around a large cylinder. The cylinder was placed in a tank containing a weak solution of salts (the dialysate). The patient’s blood was passed through the cellophane tube. The walls of the cellophane tube acted as a semipermeable membrane. The slats in the construction of the cylinder were of wood. Six hours were required for the treatment. Fluid was removed by increasing the osmotic pressure of the dialysate fluid by the addition of sugar, which increased the pressure on the membrane. This would occasionally result in rupture5.
In 1945, after WWII, Kolff’s technique was used more widely, particularly in Sweden and the USA. Kolff was invited to take his artificial kidney to New York and the first successful dialysis in Mount Sinai Hospital was in January 1948. Eight hours after the first dialysis using the Kolff machine, the patient passed urine. The treatment had been a success. Further reading on Kolff can be found here. In later years, the rotating drum was modified to become easier to use. For example, the drum was made of stainless steel and a tensioning device was used on the cellophane membrane as it had a tendency to stretch during use. These improvements paved the way for wider acceptance and use of dialysis treatment6.
In October 1956, the Kolff system became commercially available, so the lack of availability of equipment could no longer be used as an excuse for non-treatment of patients. Centres purchased the complete delivery system for around $ 1200 and the disposables necessary for the treatment were around $ 60. The system was still mainly used for reversible acute renal failure, drug overdose, and poisoning.
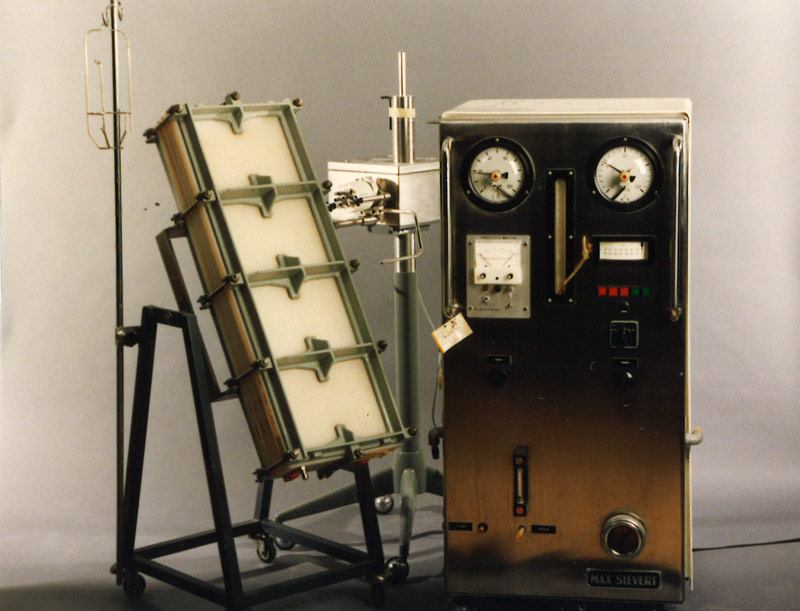
In the late 1950’s Fredrik Kiil of Norway developed a parallel plate dialyser, with a large surface area (1 m2) requiring a low priming volume. A new cellulose membrane, Cuprophan, was used and this allowed the passage of larger molecules, which until then, had not been previously available. The Kiil dialyser could be used without a pump, as the system used the patients’ own arterial pressure. This dialyser was widely used because the disposables were relatively inexpensive compared to other dialysers at that time.
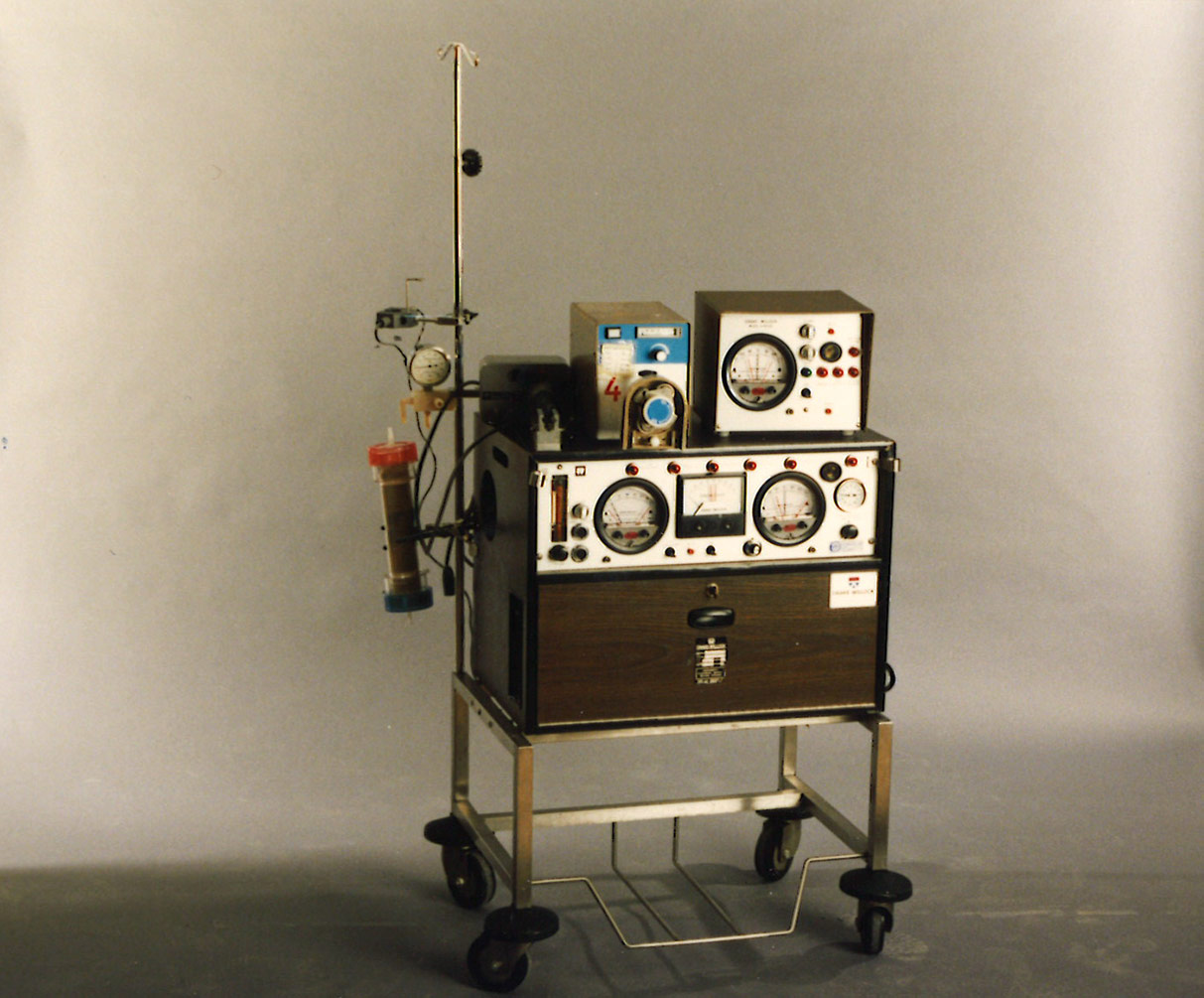
Photographs of the Kolff drum, Kiil dialyser and other machinery used in the early days of dialysis can be seen here. Before the development of the arterio-venous shunt by Dr. Belding Scribner and his colleagues in 1960, repeated dialysis for end-stage kidney disease was not really an option. Moreover, it was Scribner and his team who adapted the Kiil dialyser for use in treatments that were dependent on arterial pressure without the need of a blood pump.
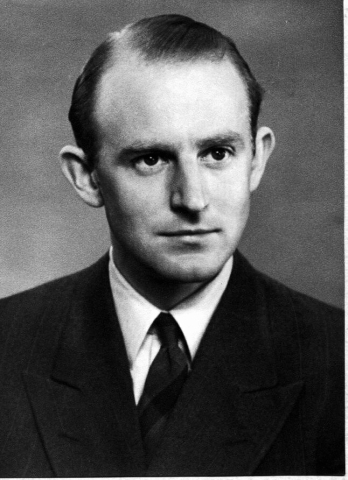
Dr. Stanley Shaldon reported in 1961 that a patient dialysing at the Royal Free Hospital in London was able to self-care by setting up his own machine, initiating and terminating dialysis; so home HD in the UK became possible. The shunt was created in the leg for vascular access, to allow the patient to have both hands free for the procedures. Dr. Shaldon reported the results of his first patient to be have overnight Home HD in November 1964. With careful patient selection, the venture was a success7.
2.1.1 The beginning of home haemodialysis
Dr. Stanley Shaldon reported in 1961 that a patient dialysing at the Royal Free Hospital in London was able to self-care by setting up his own machine, initiating and terminating dialysis; so home HD in the UK became possible. The shunt was created in the leg for vascular access, to allow the patient to have both hands free for the procedures. Dr. Shaldon reported the results of his first patient to be have overnight Home HD in November 1964. With careful patient selection, the venture was a success7.
2.2 The story of the pioneers of early Home Dialysis
In February 2017, a group of staff who were involved in the early days of dialysis came together to recall their experiences.
2.2.1 The roles of Staff
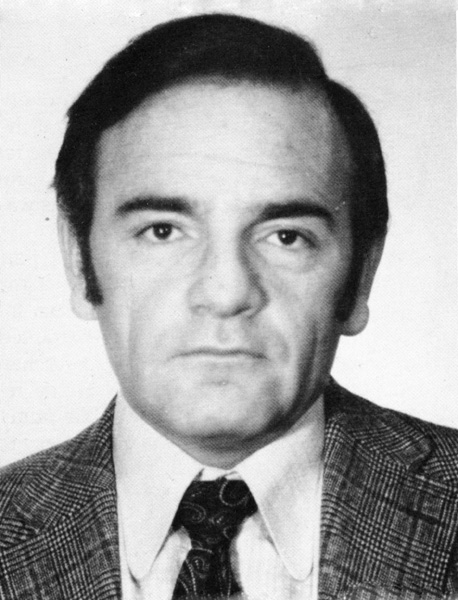
Dr. Rosemarie Baillod, who worked alongside with Dr. Shaldon, explained how the machines were developed:
“I had to develop alarm systems and I had to go to a shop called Radio Spares, and I had to buy relays, light bulbs and little alarms we got some monitoring from Cambridge Monitors – if the pressure went too high it would alarm, if it went too low it would alarm, and it was in a box about 2 feet square, it looked very smart. The first time we arrived at the patient’s home – everything leaked!”
“We did not originally have flow meters, so when you wanted to know how much dialysate we were running, we were aiming at 500 mls/min, we took a stop watch and a plastic jug and timed it, and then you adjusted pressure valves accordingly. We got Cambridge Instruments to start making machines and we were also in touch with the people in the States, Milton Roy they were called and the machines were beautifully designed. It (the machine) was supposed to look like a television.”
Dr. Baillod also explained how patients were selected at the Royal Free Hospital, London.
“I used to have to go and present 4-6 people every month from different hospitals…..I would get telephone calls and then meet the patient and family…..I would then have to present each case to a selection board…. dialysis would never have existed if we did not push the borders as we did at the beginning.”
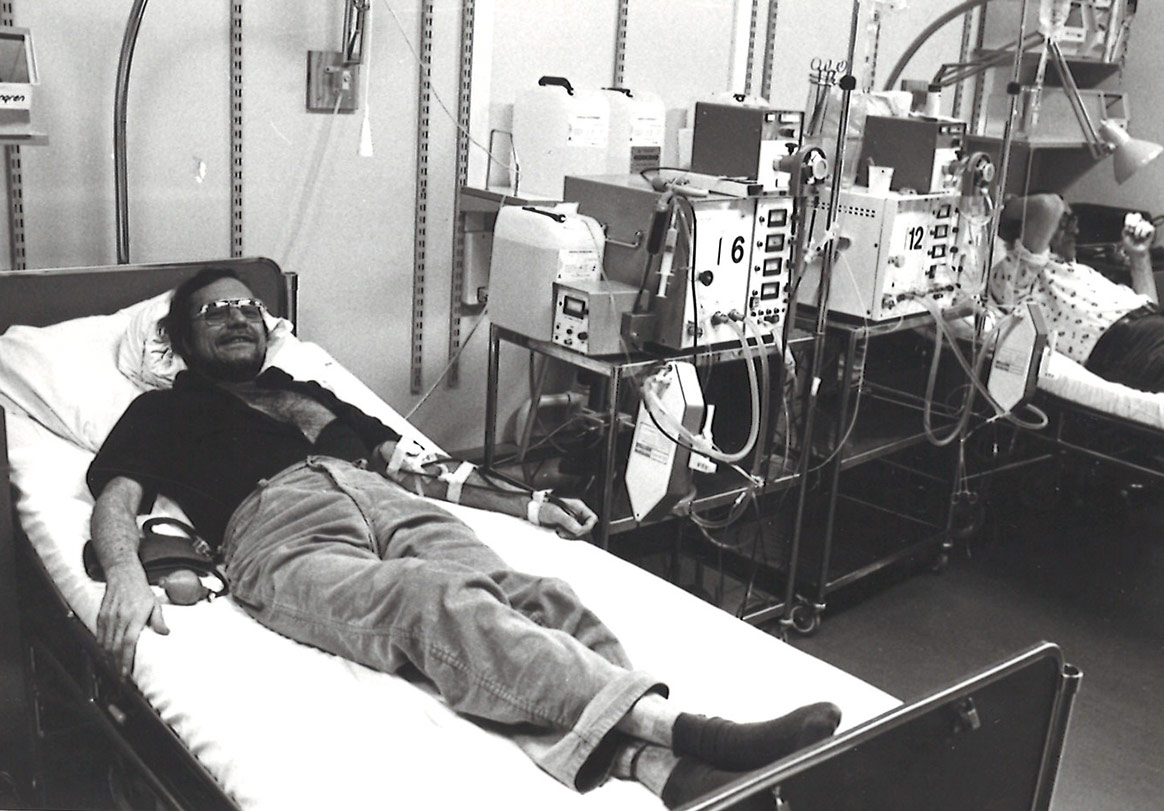
From these beginnings, large home HD programmes developed in the USA and in the UK, thus allowing expansion of the dialysis population without the need to expand hospital facilities. Many patients could now be considered for home treatment, often with surprisingly good results. The dialysis treatments could now be individualized to fit the needs of the patient, rather than the patients conforming to a set regimen.
2.2.2 The Patient focused experience
Often though, it was very difficult for patients, as Sally Taber explains
“The patients had a cooked breakfast, but during the day had to have a whole cup of jam and a whole cup of cream….if they did not eat it, we had to put a tube down.”
Ann Eady, a nurse who also cared for her husband on home dialysis, said:
“It is hard work…you are constricted, but there are benefits….you can travel, and the well-being of patients was vastly increased.”
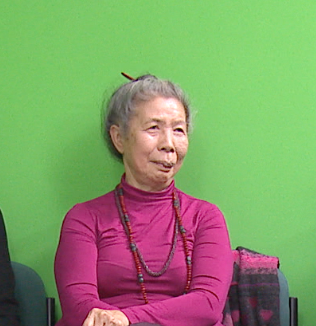
Joy Foo, explained how the training patients was very satisfying:
“We are nurses and we taught people from the street, who knew nothing about medicine and we send them home….that was the most rewarding part.”
Lesley Pavitt remember it in a similar way and recalls...
“...the patients had things (dialysis) done to them for months and years in other hospitals and then they came to us and we were able to give them the skills to take control of their life again..…and that is an incredibly empowering thing.”
2.2.3 The role of the Nurse and EDTNA/ERCA
Marcelle de Sousa describes how the nurse’s role in the renal unit was autonomous.
“If every nurse had the opportunity to work in a renal unit, I tell you, it is the making of them, you feel pride in what you do, and it is the one place that you are autonomous.”
The role of EDTNA/ERCA in the development of home dialysis across Europe was also very important, and as Sally Taber recalls taking part in a EDTNA/ERCA conference in 1975 in a debate ‘Home dialysis or not?’ which enabled sharing of ideas.
Marcelle de Sousa summarises the role of EDTNA/ERCA by saying:
“It was a fantastic forum for us…and you felt you were leading the way…..it was a great feeling.”
2.3 Case study: the Stockholm experience
Haemodialysis started in 1964 at St Eriks hospital in Stockholm. In 1967 the first patient went home. This relieved pressure on staff and dialysis beds. By 1976 the home population had grown to 40 patients with specially employed technical support. In 1979 the option of using a ’self-dialysis unit’ in an apartment became available in Stockholm for those unable to take a machine home.
Drake Willock machines, imported from the USA, were used at home from the start until the 1980’s. They had a sophisticated system to mechanically mix the concentrate and a suction pump to manage the ultrafiltrate. Ultrafiltration was not accurate. Concentrates were acetate based and often made dialysis patients quite sick by the end of treatment. Formaldehyde, a toxic chemical, was used to disinfect after each treatment. During this era, to save costs, dialyser and blood line reuse with formaldehyde sterilisation was also tried, but this practice caused allergies amongst other issues, so was short-lived in Stockholm and in most other countries.
Reddy was another commonly used machine in this era which Stockholm patients used for holidays. It only used 6 litres of water and relied on a charcoal adsorbent cartridge to remove the uraemic toxins. Bicarbonate dialysate was a major breakthrough in the 1980’s, reducing the episodes of vomiting and cramps while on dialysis. More machine options became commercially available at this time. In the 1990’s the process of ultrafiltration became more sophisticated. Improvements in technology has certainly improved outcomes during HD, but has not necessarily increased the numbers of patients at home in many countries worldwide.
2.4 Further development of dialysis in the 1970’s and 1980’s
In the early 1970’s the overall number of patients on RRT increased as awareness of the availability of treatment increased. Free-standing units for the sole use of kidney dialysis came into being, leading to dialysis becoming a full-time business. Committees for patient selection were disbanded.
However, with the development in the late 1970’s and early 1980’s, of Continuous Ambulatory Peritoneal Dialysis (CAPD) it became the first choice for Home Dialysis treatment. As a result the use of Home HD steadily declined.
2.5 The 1990’s to the present day
In the 1990’s, the number of patients on Home Haemodialysis continued to decline. The National Institute for Health and Clinical Excellence (NICE) published guidance in 2002 on home versus hospital haemo dialysis8 and recommended all suitable patients should be offered the choice between home haemodialysis or haemodialysis in a hospital/satellite unit.
Today there are wide variations in the use of Home HD. The US Renal Data System in 20169 reported that 88.0% of patients in the USA received in-centre HD, and 1.8% had Home HD. In an earlier USRDS report, the prevalence of Home HD was 15.6% for New Zealand and 9.4% for Australia, with Denmark reporting 4.6%, Finland 4%, Sweden 2.8%, Netherlands 2.4% and UK 2.1%.
Learning Activity
- When was the term ‘dialysis’ first used?
- What was the name of the doctor who developed the rotating drum dialyser?
- What did a Kiil dialyser look like?
- When was ‘NICE guidance for Home HD’ published?
- What percentage of patients in the USA today are doing Home Haemodialysis?
Acknowledgements
I would like to thank Gunnar Malmström for the information and photographs provided for the Case Study.
Further reading
Baillod, R (1975) Review of 10 years home dialysis
Thomas, N (2014) Chapter One The History of Dialysis and Transplantation in Renal Nursing 4th edition. Oxford: Wiley Blackwell
Cameron, S (2002) History of the treatment of renal failure by dialysis. Oxford: OUP
Photographs of the Kolff drum, Kiil dialyser and other machinery used in the early days of dialysis can be seen here.
In 1945, after WWII, Kolff’s technique was used more widely, particularly in Sweden and the USA. Kolff was invited to take his artificial kidney to New York and the first successful dialysis in Mount Sinai Hospital was in January 1948. Eight hours after the first dialysis using the Kolff machine, the patient passed urine. The treatment had been a success. Further reading on Kolff can be found here.
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org