







Kalliopi-Anna Poulia
Dr, MSc, PhD
Clinical Nutritionist-Dietitian
Laiko General Hospital of Athens, Greece
lpoulia@gmail.com
10.0 Dietary Management in Home Haemodialysis
Learning Outcomes
- To understand the importance of nutrition in patients undergoing HHD
- To identify the nutritional needs of a patient with CKD stage 5
- To identify the differences between the nutritional needs of a patient undergoing more frequent HHD in comparison with the conventional haemodialysis
- To identify how common nutritional problems can be managed in patients undergoing HHD
Introduction
Dietary intervention is of high importance for patients with Chronic Kidney Disease (CKD), both for disease outcome and for prevention or treatment of malnutrition (over- and under-nutrition), which is quite common in CKD patients. Malnutrition is a general term that indicates a state of nutrition in which a deficiency or excess (or imbalance) of energy, protein, and other nutrients causes measurable adverse effects on tissue/body form (body shape, size and composition) and function, and clinical outcome1. The first and most important type is Protein-Energy Malnutrition (PEM) or Protein-Energy Wasting (PEW), which is defined as a lack in supply of sufficient energy or protein to meet the body’s metabolic demands2. The causes for malnutrition are:
- An inadequate food intake secondary to anorexia caused by uremia and altered taste sensation.
- Increased demands due to disease or acute illness.
- Impaired ability to prepare food.
- Unpalatable prescribed diets (low salt, fluid restriction, low potassium, low phosphorus).
- The dialysis procedure itself due to nutrient losses (protein peptides, water soluble vitamins, etc.).
- Hypermetabolism due to chronic inflammation.
- Endocrine disorders due to uremia3,4.
Therefore, a detailed nutritional assessment is of paramount importance in providing optimal care to individuals with CKD of all disease stages. Classically, three major lines of inquiry, i.e. biochemical measures, dietary intake, and body composition, are used to assess the protein-energy nutritional status.
Protein intake is of major importance, as protein loses occur during HD. Sufficient intake of high biological value proteins should be included. At the same time, phosphate control necessitates the correct use of phosphate binders. Moreover, sodium restriction is necessary to control thirst and fluid intake and facilitate better blood pressure control. Finally, potassium control is of major importance, achieved mainly by the restriction of potassium rich food choices, mainly from the food groups of fruits and vegetables.
The dietary management of patients undergoing Home Haemodialysis (HHD) depends on the type of haemodialysis the patients follow. For the patients following a three-times four hours per week HHD programme, dietary restrictions remain the same as conventional HD. By increasing the frequency and the duration of haemodialysis at home (Short Daily Haemodialysis (SDHD) or Nocturnal Haemodialysis (NHD)) we increase the quantity of waste products removed from the patients’ body. Therefore, most of the restrictions existing for conventional HD can be reduced.
10.1 Biochemical control with more frequent haemodialysis
Due to the high prevalence of malnutrition after the initiation of HD a baseline measurement is useful for monitoring of nutritional status. At the beginning of HHD nutritional status may be already negatively influenced by the dietary restrictions of conventional HD or even by the adherence in restrictive dietary plans in earlier stages of CKD.
Unintentional weight loss, which reaches 5% of body weight in 3 months, is considered a significant weight loss and should be an alert for action in order to prevent malnutrition.
Moreover, limited appetite, low phosphorus, cholesterol, and albumin levels should be detected early and patients should be encouraged to increase their energy and protein intake.
According to available research data, after only a few weeks of the initiation of Frequent Home Haemodialysis (FHHD) appetite increases and food intake also improves, resulting in the increase of albumin levels and an improvement of the nutritional status5,8. Nonetheless nutritional status should be monitored closely in patients undergoing as early detection of alterations in nutritional status is important for the early treatment of malnutrition according to Table 10.1.
Guidelines can vary a little and each unit will choose which guidelines to follow. According to KDOQI Guidelines for CKD Care9 serum albumin <4 g/dl, pre-albumin <30mg/dl, pre-dialysis creatinine <10 mg/dl and cholesterol <150 mg/dl are clinically useful markers indicating high possibility of protein-energy under-nutrition in CKD patients, whereas the International Society of Renal Nutrition and Metabolism recently included serum albumin <3.8 g/dl as one of three biochemical diagnostic criteria for protein-energy wasting (among transthyretin and cholesterol levels)10. Moreover, according to EBPG Guideline on Nutrition11 BMI should be >23 kg/m2 in maintenance haemodialysis patients. These parameters should be monitored regularly, i.e. on a monthly basis, to assess the nutritional outcomes and needs of the patients.
Table 10.1: Suggested strategies to monitor nutritional status and guide therapy in advanced CKD12.
| Simple (monthly) assessment | Findings | Possible interventions |
| Body weight/ Ideal Body Weight Serum albumin Serum creatinine |
Continuous decline or <85% IBW <4.0 g/dl Relative low pre-dialysis values |
Suspect PEW and perform detailed nutritional assessment Consider preventive measures |
| Detailed early assessment | Findings | Possible interventions (simple) |
| Serum prealbumin Serum transferrin Lean body mass and/or fat mass SGA |
<30mg/dl and/or <200mg/dl and/or Unexpected decrease Worsening |
Dietary counseling: Protein intake 1.2g/kg/d, energy intake 30-35 Kcal/day Increase dialysis dose to Kt/V>1.4 Use biocompatible membranes Upper Gl motility enhancer |
| Repeat detailed assessment (2-3 months from previous) | Findings | Possible interventions (more complex) |
| Serum prealbumin Serum transferrin Lean body mass and/or fat mass C-reactive protein |
<30mg/dl and/or <200mg/dl and/or Unexpected decrease >10 mg/l |
Nutritional support (Oral nutritional supplements, enteral nutrition, IDPN if needed) Anabolic factors Appetite stimulants (experimental Anti-inflammatory (experimental) |
10.2 Nutritional intake – less build up results in more dietary freedom
Due to the increased frequency of dialysis, FHHD can provide a more “physiological” function for the patients, allowing them to excrete waste products of metabolism more efficiently. Consequently, the restrictions applied to patients undergoing conventional HD, mainly for the control of electrolytes, i.e. phosphate and potassium, and the restriction on fluid control may be reduced, according to the patient’s serum blood results. Recently FHHD patients in KIHDNEy cohort showed stable mineral & bone disorders parameters with fewer dietary restrictions, more patients were in the phosphate target range and had significant improvement in bicarbonate levels from baseline24.
Nutritional intake can be measured in calories for energy or in grammes for proteins, usually expressed per kilogramme of body weight per day (kcal/kg/day or g/kg/day).
10.2.1 Energy intake
Sufficient energy intake is essential in order to achieve a positive nitrogen balance. An energy intake of 35 kcal/kg/day is associated with better nitrogen balance and is recommended in stable CKD patients in the range of ideal body weight ±10%13. The recommended energy intake in a clinically stable chronic HD patient is 30–40 kcal/kg/ day, adjusted to age, gender and to the best estimate of physical activity level. For patients >60 years old or obese, energy intake prescription should not exceed 30 kcal/kg/day9,11,14.
Overweight or undernourished patients may need adjustments of energy supply, to ensure better coverage of their needs. Energy intake for patients > 60 years old should be 30 kcal/kg/day due to their reduced energy needs if they have a more sedentary life due to ageing9. However, regular physical activity should be encouraged as it helps in maintaining the functionality of muscles and improves endurance and cardiovascular health.
10.2.2. Protein intake
Protein needs in patients on maintenance HD exceed the needs of normal healthy people as the dialysis treatment itself induces significant nutrient losses, particularly amino acids, oligopeptides, water soluble vitamins and trace elements. Moreover the dialysis procedure is a catabolic one, inducing catabolic stress and release of proinflammatory cytokines, which raise the protein needs15.
According to the available guidelines;
- The recommended protein intake is 1.0 -1.5 g/kg/day in clinically stable chronic haemodialysis patients and nPNA at least 1.0 g/ body weight/day.
- The optimum protein intake for a maintenance dialysis patient who is acutely ill is at least 1.2 to 1.3 g/kg/day4,11.
- More specifically, for patients on HHD, protein requirements are of great importance as the increased frequency of dialysis increases the protein losses.
Therefore, the higher level of recommendations should be applied for patients undergoing FHHD. Generally, it has been reported that protein intake improves after the increase of the frequency of dialysis, with a subsequent increase of phosphate intake, without altering phosphate blood levels, even with potential reduction in phosphate binders use16. Nonetheless, protein intake is of major importance and should be monitored closely to ensure sufficient coverage of the patients’ needs.
Protein intake should be of high biological value, i.e. from animal sources, e.g. poultry, meat, egg whites, soya, cream cheese, etc. On FHHD animal protein high in phosphorus (small fish, dairy products, cheese, meat close to the bones) can usually be more liberally consumed, compared to conventional HD, as the waste products of protein metabolism are excreted more efficiently. In case of poor phosphate control, the consumption of high phosphate protein food items should be limited, and protein should be taken only in the meals when the patient is taking phosphate binders, in order to directly limit phosphorus absorption from the gut.
If alteration in taste of animal protein is reported (metallic taste), alternative sources of high biological value protein should be given. Fortification of food with protein supplements could be a way to provide increased protein.
10.2.3. Fat intake
CKD raises the risk of developing cardiovascular disease17, due to inflammation, disturbed calcium to phosphorus ratio and pre-existing risk factors such as diabetes mellitus. Therefore, all the nutrition related cardiovascular risk factors should be taken into account18,19. In HD patients, emphasis should be given to the quality of their fat intake;
- Saturated fat should be limited to <10% of total energy intake.
- Cholesterol <250 mg/day.
- Monounsaturated should be 10-20% of Total Energy Intake (TEE).
- Polyunsaturated fat should provide around 10% of TEE.
Therefore, sources of saturated fat, such as full fat dairy, cheese, fatty meat, poultry with skin, fried food, butter and full fat cream should be avoided, while olive oil intake should be one of the main sources of fat. Emphasis should be given in ω-3 fatty acid intake, which could be a part of the dietary plan in patients undergoing HHD with increased frequency or duration, due to better phosphate levels control. Fatty fish intake, such as cod or salmon could be included at least once a week, with the correct use of phosphate binders in patients with poor phosphate control.
10.2.4 Vitamins and trace elements
Dialysis patients are prone to developing vitamin deficiencies due to abnormal renal metabolism, inadequate dietary intake and compliance to strict dietary restrictions, loss of gastrointestinal absorption and dialysis losses. Losses depend on the type of dialysis and its duration, since high-flux and high-efficiency dialysis attenuates losses in water soluble vitamins. Vitamin deficiencies develop slowly but they can affect patients’ quality of life. Each patient’s vitamin status should be evaluated on an individual basis, according to the age, gender, dietary intake, dialysis losses, residual renal function and type of dialysis before he is subscribed to any supplemental vitamin therapy11. Blood vitamin levels, alongside with early detection of symptoms of vitamin deficiencies is important to assure the individualization of treatment.
10.2.4.1 Water soluble vitamins
During haemodialysis, a significant amount of vitamins are lost in the dialysate. In conventional HD, due to potassium dietary restrictions in vegetables and fruits, patients are particularly prone to deficiencies in folic acid and vitamin C. Folic acid intake (1mg-5mg) is needed for the prevention of hyperhomocysteineamia. Vitamin C should also be taken as a supplement (75-90 mg) although this is most important in those restricting their vegetables and fruits11.
Thiamin deficiency is common in haemodialysis patients as it is readily removed by HD and at the same time dietary intake is often inadequate. Dietary sources of thiamin include seeds, legumes and pork. Beriberi is the most known condition caused by thiamin deficiency, while other manifestations include neurological symptoms (Wernicke encephalitis). Currently all the vitamin supplements for renal patients include thiamin11.
Rivoflabin deficiency is not common, even though it is well cleared during a haemodialysis session, as its main sources include lean meat, eggs, food cereals and bread, food items included in end stage CKD patients’ diet. B6 needs can be elevated by the accelerated erythropoiesis by erythopoetin use. B12 is necessary for the prevention of pernicious anaemia and for an optimal folic acid metabolism. It is found in sufficient amounts in meat, milk and egg yolk, while supplemental use is safe in renal patients intake is usually close to DRI11.
The recommendations for vitamin intake and supplements for haemodialysis patients are summarized in Table 10.2. There are no specific recommendations for patients undergoing FHHD and further research is needed in order identify the differences in vitamin needs for HD patients in different types and frequency of treatment.
10.2.4.2 Fat soluble vitamins
Fat soluble vitamins should be treated with caution, as they are stored in the body and the toxicity risk is higher. Vitamin A deficiencies are rare in renal patients as it is not removed by haemodialysis. Therefore, the danger of toxicity is higher and supplemental use is not recommended. Daily needs can be covered by dietary sources which include dairy products, fish oil and carrots. Concerning vitamin K, there is no evidence of deficiencies in CKD patients receiving sufficient dietary intake11.
Table 10.2. Recommended dietary intake and supplements of vitamins11
| Vitamin | Daily recommendations |
|---|---|
| Water soluble vitamins | |
| Thiamin (B1) | 1.1-1.2 supplement |
| Riboflavin (B2) | 1.1-1.3 supplement |
| Niacin (B3) | 14-16mg supplement |
| Pantothenic Acid (B5) | 5 mg supplement |
| Pyridoxine (B6) | 10 mg supplement |
| Biotin (B8) | 30 μg supplement |
| Folic Acid (B9) | 1-5 mg supplement |
| Cobalamine (B12) | 2.4 mg supplement |
| Vitamin C | 75-90 mg supplement |
| Fat Soluble vitamins | |
| Vitamin A | 700-900 μg intake - no supplement |
| Vitamin K | 90-120 μg - no supplement |
| Vitamin E | 400-800 IU supplement for secondary CVD prevention and cramps |
10.2.5 Electrolytes and minerals
10.2.5.1 Sodium and fluids
Sodium restriction is indicated for all stages of CKD as it is essential for the control of the extracellular volume and for better control of arterial blood pressure. In HD, sodium control is even more important, as it facilitates compliance with fluid restrictions and prevents interdialytic weight gain in anuric and oliguric patients, given that it reduces thirst. Salt substitutes containing potassium chloride should be avoided in HD patients. Salt can be substituted by the use of herbs and spices. More specifically, sodium should be restricted to no more than 80-100 mmol (2000-3000 mg) or 5-6 g (75 mg/kg/day).
Fluid intake, is generally more liberal in patients using FHHD at home because more fluids are removed over the week.
Therefore, many patients can exceed the limit of 500-1000 ml in addition to daily urine output. No strict recommendations exist for fluid intake for patients on FHHD, but the aim is to control interdialytic weight gain11.
In cases of patients who find it difficult to control their fluid intake all foods that are liquid at room temperature (18-20°) should be counted as fluid, except oils. Thirst control can be facilitated by reduction in salt intake, the consumption of chilled liquids, consumption of ice cubes instead of water, addition of lemon in water and the use of chewing gums to hydrate mouth20,21.
10.2.5.2 Potassium
In healthy subjects, 90% of dietary potassium is excreted by the kidneys. For those on dialysis limiting dietary intake and adequate dialysis can achieve acceptable potassium levels. Potassium exists in almost every food item so severe restrictions should be limited, in order to ensure a balance in patients’ diet and quality of life.
In the majority of patients undergoing increased frequency HHD, potassium levels are maintained more easily within normal levels. Therefore, the diet can be more liberal, in terms of fruit and vegetable consumption. Fiber intake is also easier to maintain within the recommended amounts, facilitating the prevention of constipation. In CKD patients, potassium intestinal excretion is increased as a compensatory mechanism and the prevention of constipation also contributes to the prevention of hyperkalemia.
Hyperkalemia causes nausea, weakness, numbness or tingling, slow pulse, irregular heartbeat, and a high risk of heart failure or sudden death. Following any of these signs serum potassium levels should be measured and documented before HD. In patients with pre dialysis potassium >6mmol/l, daily potassium intake should not exceed 50-70 mmol (1950-2730 mg) or 1 mmol/kg/day11. If potassium levels are repeatedly elevated, patients should be advised to reduce their potassium intake, by avoiding fruits and vegetables rich in potassium (bananas, oranges, potatoes, tomatoes, etc.) and choosing lower potassium ones (apples, pears, lettuce, carrots, boiled vegetables, pealed fruits or boiled and chopped).
Table 10.3. Steps to Calculate the initial binder prescription22.
| Step | Example | Example |
|---|---|---|
| Phosphate intake | Total dietary P intake | 1000 per day or 7000/week |
| Amount absorbed (50-70% of mixed diet in non-renal (53% renal vs 77% in non-renal) |
Dietary intake multiplied by 50-60% absorbed | 600 per day or 4200/week |
| Average HD/PD clearance HD = 800 per treatment PD = 300-315 per day |
Amount abs - dialysis clearance = remaining P to be bound by phosphate binder | HD: 4200-2400 = 1800 mg P/wk or 257 mg/day PD: 4200-2205 = 1995 mg P/wk or 285 mg/day |
| Divided by estimated binding power or the binder of choice | Remaining P/binding power | 257/39 (approx. P bound by 1g CaCO3) = 6.5 g CaCo3 257/45 (approx. P bound by 1g calcium acetate)= 5.7 g 257/15-30 (approx. P bound by 1 Al(OH), tablet= 12-17 tablets 257/64 (approx. P bound or 800mg sevelamer HCI) = 4 tablets 257/32 (approx. P bound per 400mg sevelamer HCL) = 8 tablets Note: Calculations for OD would use 285 instead of 257 |
Note: The above table estimates the initial prescription based on average phosphorus absorption, average dialysis clearance and the approximate binding potential for the binder of choice. The dose should be monitored and adjusted based on response of the individual patient.
10.2.5.3 Phosphate
Hyperphosphataemia is related to hyperparathyroidism, calcification and mineral bone diseases. Therefore, serum phosphate should be closely monitored. In patients undergoing HD, their high needs for protein can lead to phosphorus accumulation, as each HD session only removes 500-700 mg of phosphate. Protein foods provide 12-16 mg of phosphate/g, while dairy products have the highest content11. Selection of protein foods with the lowest content of phosphorus can help in achieving the phosphate goals, without affecting protein intake.
As frequency of HD is increased, phosphate levels can be maintained within the normal levels more easily, and therefore the patients are allowed to follow a more liberal dietary plan. In patients who do not achieve their phosphate levels goals, the appropriate use of phosphate binders – type, dose and time – will increase phosphorus excretion. In Table 10.3 the steps to calculate the initial binder prescription are described for conventional HD and in table 10.4 the main phosphate binding compounds are listed. It is important that phosphate control should not compromise protein intake. According to the existing nutritional guidelines, phosphate intake of 800-1000 mg or <17mg/kg/day is recommended4,11.
Nocturnal Home Haemodialysis (NHHD) removes about 5638 mg of phosphorus per week, attributed to the increased frequency and long duration of dialysis. This fact liberates the diet of the patients who can control their phosphate levels with minimal or no use of phosphate binders. Short Daily Home Haemodialysis (SDHD) removes somewhat more phosphate than Conventional HD; however, the improved appetite seen in SDHD patients and consequent increased protein and phosphorus intake usually leave patients in a net positive phosphate balance23. In case of hyperphosphatemia the use of phosphate binders should be considered.
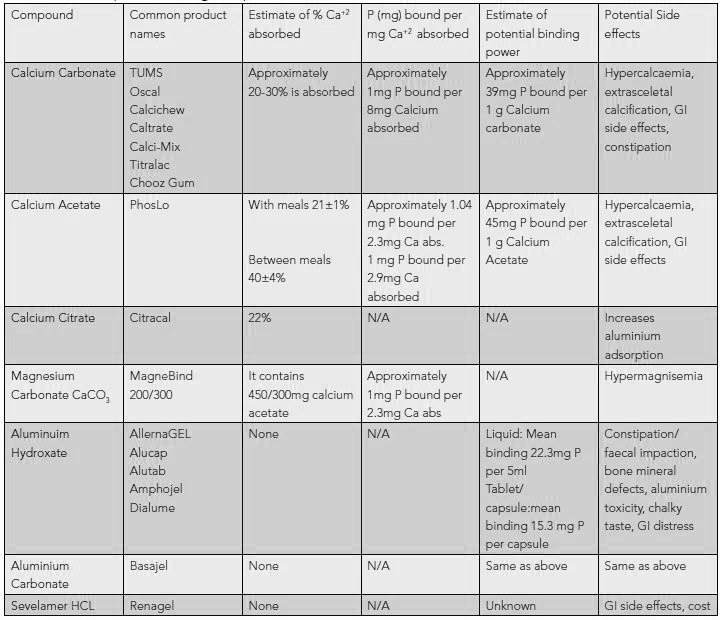
In Table 10.4 the main phosphate binding compounds are presented.
Table 10.4. Phosphate binding compounds22.
Summary
Nutrition is very important for people on FHHD although more dialysis means less restrictions. Potassium, phosphate, fluid, protein and vitamins are all important elements. Every patient should receive tailor made information based on their daily needs, food preferences and blood results.
Learning Activity
- What are the main causes of malnutrition in CKD patients?
- Which biological markers should be monitored for the early detection of malnutrition during haemodialysis?
- What are the energy needs of patients undergoing HD?
- What are the protein needs for the patients undergoing frequent HHD?
- Describe 5 differences to the diet of a patient when they move from conventional to frequent Home Haemodialysis.
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org



