
Dr María F. Slon Roblero
MD, MSc.
Consultant Nephrologist
In charge of the Home Dialysis Program at the Complejo Hospitalario de Navarra, Spain
mf.slon.roblero@navarra.es

Jane Golland
RN, MA Deputy Head Nurse of the Hemodialysis Department, Galilee Medical Center, Naharia, Israel
jane.golland@edtnaerca.org
4.0 Basics of Home Haemodialysis
Learning Outcomes
- Identify appropriate patients for HHD
- Understand different options for HHD prescriptions and the benefits of frequent dialysis
- Learn what a Dosing Calculator is and how to use it
- Understand appropriate anti-coagulation use during HHD
- Gain knowledge about optimal vascular access for HHD, benefits and various cannulation techniques
- Understand the technical aspects necessary for successful implementation of HHD
- Understand the steps necessary for successful implementation of HHD
Introduction
Home Haemodialysis (HHD) is an ideal treatment option for suitable patients requiring renal replacement therapy (RRT). There are challenges involved in the successful implementation of HHD. Appropriate advance planning of the home infrastructure and environment, suitable patient education, finding the appropriate regimen of treatments, home visits schedule and ongoing support to patients and their family members help ensure a smooth start and the continual success of HHD over a long period.
This chapter provides evidence based recommendations for the successful planning of the process, from the identification of suitable patients until the start of independent HHD.
4.1. Target population for Home Haemodialysis
4.1.1 Capacity to perform HHD skills
Most patients are suitable for HHD. Basic requirements include: adequate manual dexterity and vision, reading and writing skills, home equipment, initiative and motivation1. Patients lacking in some of these requirements may still be appropriate for HHD with a care partner or paid helper who meets these requirements and will assist during each treatment. Age is not a barrier either, there are many older patients who are capable of learning and undertaking self-care dialysis techniques, though a longer training period may be necessary2. KIHDNEy European cohort reported that any access is feasible at home and a wide range of patients may be suitable for HHD regardless of age (from 15 to 84 years), size (BMI from 13.3 to 50.8) and commorbidities (Charlson average score 3.9, up to 11)47.
4.1.2 The benefits and indicators for HHD
HHD empowers patients with independence and control over their health care. It reduces the time required traveling to dialysis centers, allows greater flexibility in scheduling, and has the potential to reduce the dietary restraints required of dialysis patients3.
Some populations who may benefit from HHD include:
- Patients upon failure of peritoneal dialysis who need to transfer to HD – these patients are used to performing dialysis at home, already have the set up and storage space, and often prefer to continue with the flexibility and independence of self-care.
- Patients after transplant rejection, who are often younger, healthier and more independent; patients holding jobs or regular activities, who need a flexible schedule and more freedom during daytime work hours4,5,6.
- Complex patients, for example those with severe obstructive sleep apnea, refractory hyperphosphatemia, persistent uremic symptoms, difficult to control hypertension and refractory extracellular fluid overload often benefit from home treatment modalities7.
- Special medical requirements as Frequent HHD (FHHD) improves some clinical and quality of life outcomes such as successful deliveries for pregnant patients, bed-side dialysis for untransportable or hospitalised patients, unplanned start recovery, end of life palliative care.
- KDOQI guidelines state: “During pregnancy, women with endstage kidney disease should receive long frequent hemodialysis either in-center or at home, depending on convenience” 48.
- Moreover complex patients may specifically benefit from receiving more Frequent Home Haemodialysis (FHHD), e.g. improving blood pressure control and reducing the risk of intradialytic hypotension49,50 (see Chapter 3).
Emergency initiation of dialysis treatments is not necessarily a barrier for successful implementation of HHD. Despite the lack of an informed choice at the initiation of the emergency treatment, even a patient with a suboptimal start in HD can be successfully transferred to HHD after appropriate education and training8,9,10.
4.1.3 Maximizing uptake
All target population groups and their caregivers need to be activated and empowered in order to consider home dialysis as a treatment modality. A strong emphasis must be placed on the development of patient-focused educational programs and resources to meet patients’ individual needs.
An integral part of shared decision making is development of a programme that meets the health literacy and cultural needs of patients and caregivers. This may enable HHD as a treatment option for most patients11,12. Pre-Dialysis Education Programme (PDEP) should discuss all odalities and involve renal professionals and patients advocates for each. Awareness days or events are usually very successful to inform patients already on dialysis who may want to experience FHHD benefits. In the KIHDNEY European cohort, 61% of HHD patients come from in-centre, 9% from PD, 7% from transplant. Only 17% are incident patients47.
Extending the duration of HD sessions can improve clearance of middle sized molecules and larger solutes, normalize serum phosphorus and provide adequate fluid volume control with lower ultrafiltration rates; but an excessive approach can lead to hypophosphatemia and more rapid loss of residual renal function14,15,18,19,20,22.
4.2. Home Haemodialysis therapy options
4.2.1 Schedule and prescription
Home Haemodialysis therapy allow the nephrologist and patient the opportunity to tailor the best self-care therapy for the patient’s current health and lifestyle13. The principal advantages of dialyzing at home is the flexibility of scheduling treatments, the possibility of more intensive HD and the possibility to incorporate the treatments into the patient´s lifestyle; favouring a significant improvement in patient outcomes and quality of life13,14,15,16,17,18,19.
The optimal HHD modality remains unknown, and it is unlikely that any single dialysis prescription will be optimal for all patients17,18. We should try to offer a range of alternative HHD prescriptions that can improve patients clinical and biochemical measures, normalize risk factors, improve health outcomes and best address individual needs.
4.2.2 Benefits and risk of prescriptions
There are risks and benefits to each HHD regimen. More frequent treatments have been shown to improve fluid volume and blood pressure control, with need for less blood pressure-lowering medication, to improve phosphorus removal and serum level control with fewer dietary restrictions, to reduce left ventricular hypertrophy, and to lower mortality, (see Chapter 3).
However, more frequent HHD regimens may also increase some direct costs, there is a higher risk of vascular access complications due to cannulation frequency and failure to follow aseptic technique at home. There can also be burden on caregivers.
Table 1: Home Haemodialysis therapy options
4.2.3 Choosing the best individualised option
Table 1 is an overview of various regimens: different schedules with different equipment, with the main characteristics of each prescription. Adjustments must be made per patient health status, clinical goals and individual lifestyle and preferences.
When it is necessary to increase the dialysis dose, increasing the duration and frequency of sessions is more effective than changing flow rates and/or dialyzer size13,16,18,19,20,21.
There is no single prescription that provides optimal therapy for all patients. Patient health status, clinical goals, lifestyle and preferences all influence the prescription. It is important to be aware of the potential risks and benefits of each option to the patient and care partner, and adapt the prescription when necessary to ensure longterm success.
4.3. Prescriptions for NxStage dialysis
4.3.1 Dosing Calculator
The NxStage Dosing Calculator is an online software tool, CE marked, designed to assist in prescribing haemodialysis therapy exclusively with the NxStage System One cycler. With a specified set of algorithms based on formulas documented in scientific literature, it automatically performs calculations to determine a range of appropriate treatment frequencies, treatment durations, and therapy fluid volumes, according to the specific characteristics of an individual patient, to achieve established targets23,24.
The prescription options provided by this tool can be used as a baseline for the development of a treatment plan, or can be very helpful for modifying the dialysis prescription according to changes in the condition of the patient that may require a change in the patient’s prescription over time.
| DOSING CALCULATOR | |
|---|---|
| 1. PATIENT BODY WATER VOLUME. Using either the Watson calculator or by directly entering the value in liters. To use the Watson body water calculator, we need the patient age, weight, height, and sex. (Patient must be 18 or older to use this formula) | |
| 2. TREATMENT PARAMETERS. In this section we must enter the following data directly related to the treatment | |
| Target weekly std Kt/V | This value sets the standard Kt/V that will be provided by all choices in the options table. (KDOQI Guidelines suggested a target std Kt/v of 2.3 with a minimum delivered dose of 2.1 for schedules other than thrice weekly)26 |
| Blood flow rate | This value refers to the flow of blood allowed by the vascular access of the patient. |
| Hematocrit | This value must be the patient's current hematocrit value; enter the whole number without "%" symbol. |
| Weekly UF volume | This value refers to the amount of ultrafiltration anticipated to be removed weekly, in liters. |
| Max UF rate | Establishes the maximum ultrafiltration per hour allowed (UF rates should be below 10 ml/hr/kg to improve mortality)26 |
| Min hours/week | Establishes the minimum treatment hours per week. |
| Allow 3 days per week | Yes or No. This setting includes or not, the thrice-weekly schedule choice in the options table. |
| Round up to nearest SAK | When set to Yes, the calcutlator will round up the options to 40, 50 and 60 L volumes to match the standard SAK capacities. |
| Include rinseback in daily UF | When set to Yes, this option adds 280 ml to the UF target for each treatment to account for the rinse-back volume. This improves the accuracy of the treatment time if the rinse-back volume is not included in the Weekly UF volume setting. |
4.3.2 Prescribing Frequent HHD (FHHD)
Prescription of Frequent Home Haemodialysis (FHHD) differs from Conventional Haemodialysis (CHD).
Prescription of FHHD with low dialysate volume can be summarised in 2 steps:
Step 1: Calculation of minimal cumulative hours of treatment per week based on weight gain and ultrafiltration limitation. Then time can be divided by the number of sessions per week.
Step 2: Calculation of minimal dialysate volume based on Kt/V target and Total Body Water (TBW).
Obeservational studies showed that Ultrafiltration Rate (UFR) above 13 mL/kg/h is associated with high cardiovascular morbidity and mortality and suggest UFR should be below 10 mL/kg/h25,52. A recent study showed even better outcomes with UFR below 6.8 mL/kg/h52, which is also the average UFR observed in the KIHDNEy European cohort of patients in FHHD47.
Dosing Calculator23 is a comprehensive tool on-line, CE marked, to identify a range of rescriptions for a specific patient. Input parameters required are:
- Age, weight, height and gender to calculate TBW.
- Target std Kt/V, blood flow rate, haematocrit, volume to remove per week, UFR limit and minimum hours per week.
4.3.3 How to interpret the results
Once the previous parameters have been entered, the table with treatment options will appear. This “Options table” will show different possible prescription choices, with different frequency, duration and volume of dialysate necessary in each session to meet the target of standard Kt/V based on the patients’ water volume, blood flow rate, hematocrit, and ultrafiltration parameters, complying with the ultrafiltration constraints, minimum frequency, and minimum time selected.
It must be very clear that this is only a tool to help decision making. This tool does not replace the judgment or experience of the physician or licensed healthcare practitioner to make an independent determination of the therapy best suited for an individual patient23,24.
This table of options allows flexible treatment, adjusting the dialysis prescription according to the needs of each patient and allows formulating different options related to the frequency and time of treatment, so that the patient can fit the treatment in his life and not adapting his lifestyle to the treatment. This flexibility in prescribing is an essential characteristic in home treatments, which makes a remarkable improvement in the quality of life of these patients.
4.4. Anticoagulation
4.4.1 Physiology
During HD several mechanisms activate different pathways that alter the coagulation system30,32,33. The coagulation cascade is initiated as soon as the blood is in contact with external surfaces, but also air contact and the presence of turbulent blood flow leads to activation of platelets and leukocytes, resulting in clotting of haemodialysers32,33.
Table 2: Anticoagulation options for Home Haemodialysis
Note: Even though Regional Citrate and Prostacyclin anticoagulation are valuable options for in-center haemodialysis, their used is not normally employed for home haemodialysis due to its complexity for the patient and risk of adverse events.
Abbreviations: HIT, heparin-induced thrombocytopenia; aPTTr, activated partial thromboplastin time ratio; anti-Xa, anti-factor Xa; INR, international normalized ratio; IU, international unit; HD, haemodialysis.
One more factor directly related to dialyser is the membrane biocompatibility, with a contact area of 1 to 2m2, which modifies the capacity to activate thrombotic pathways depending on the type of membrane27,30. Anticoagulation treatment is essential to prevent this phenomenon, and knowledge of basic principles of the clotting cascade30,32,33,37 may help to achieve a performance improvement in dialytic therapy, using the lowest possible dose of anticoagulant while also reaching a prudent time of haemostasis of the vascular access.
4.4.2 Determining the dose of anticoagulant
In HHD, the responsibility for anticoagulation is shared between doctors, nurses and an appropriately trained patient31. There are some important differences regarding anticoagulation between in-centre HD and HHD. While in-centre there are monitoring methods to adjust the anticoagulation dose, these methods are not available for routine use in the home environment. In HHD, we have to guide through clinical parameters to assess whether a patient is treated with the correct anticoagulation dose.
Signs that the dosing is too high include if the needle sites continue to bleed for more than 15–20 minutes after dialysis; or the dose is inadequate, if there are thrombus or if there is clotting of the circuit30,34.
4.4.3 Determining the type of anticoagulant
Another important difference between home and in-centre HD is treatment duration: as in home the prescription could be short daily or long nocturnal modality, the former would be enough anticoagulation with low-molecular-weight heparins (LMWH) and the latter normally requires unfractionated heparin (UFH), for adequate performance34. The third aspect in which both therapies differ is: the greater variety of anticoagulants affordable in the hospital setting, where citrate and prostacyclin are valid options, but are not usually extrapolated to the population on HHD, due to the complexity of the protocol and risk of adverse effects30,32,33,35.
It is important to clarify that systemic anticoagulation and/or antiplatelet therapy is insufficient to prevent clotting during HD26,27,29 but increases the risk of bleeding side effects29,30 as well as it is remarkable that no differences have been found in anticoagulation regimen between fistula and catheter vascular access27. On the other hand, KIHDNEy cohort showed that 40% of patients doing FHHD didn’t use any anticoagulation47.
In practice, there is no ‘‘standard’’ dosing for anticoagulation; rather there are several choices that can be tailored to meet individual patient needs34,35. Table 2 shows a summary of the different types of anticoagulation available and the characteristics of each for home dialysis treatment30,32,37. It is important to update this topic on a regular basis, since prevention of clotting of the extracorporeal circuit with anticoagulation is so important to the safe and effective delivery of HHD therapy30,34.
4.5. Vascular access
Proper vascular access (VA) is essential for successful home haemodialysis. All types of VA: Arteriovenous Fistula (AVF), Arteriovenous Graft (AVG) and Central Venous Catheter (CVC) can be used for HHD38,47. Despite many studies, optimal VA for HHD has yet to be defined. AVF is the preferred vascular access for Renal Replacement Therapy (RRT), as it is associated with lower rates of access-related events, compared to CVC42.
There are two common techniques used for self-cannulation with AVF: “buttonhole” and “rope ladder”.
CVC is also a possible VA for HHD. Benefits include ease of use and shorter training time. The risk of infection may be higher compared to AVF or AVG, however the correlation with morbidity and mortality have not yet been studied sufficiently for the unique population of HHD patients45.
More details about vascular access is available in the chapter on vascular access.
4.6. Setting up the Home Haemodialysis room
4.6.1 Assessing the environment and determining the right space
Many patients will dialyse in an existing room such as the bedroom or the lounge, depending on what time of day they intend to dialyse. Minor changes to power, water or drainage are often sufficient for HHD to occur with small systems designed for home. Installation of a traditional machine would involve more modifications, space and costs. It is strongly recommended that prior to the installation process a technician or home nurse visits the patient’s house.
If the patient wishes to develop a new space for dialysis or adapt an existing space it can be helpful to make a drawing and ask the patient to sign the drawing if changes are needed. If there are any structural changes (for plumbing, power or storage space) it is important that the owner of the building is notified and agrees to the changes. Responsibility for costs must be clearly determined and may vary by dialysis unit and region.
4.6.2 Basic requirements
The basic requirements at home include:
- Electricity: The dialysis machine should have 240V / 10A fuse for Class 1 equipment. Installation requiring modifications should be carried out by an electrician. Check the current regulations for your country.
- Tap water: The water should be drinking water quality according to national standards. Water pressure should be higher than 2 bar. Installaton requiring modifications should be carried out by a plumber to avoid the hazard of water leakage.
- Light: The room needs good background light. Two 75W bulbs at the ceiling and a lamp with an adjustable arm close to the patient are ideal. It’s possible to purchase a LED lamp with a magnifying screen.
- Dialysis chair: A comfortable armchair, which can lean back, with a footrest is prefered. If the patient needs a bed, an electric adjustable bed is prefered. However every type of bed may be adapted to the treatment.
- Table for Connection/Disconnection: A small table on wheels that can fit next to the dialysis chair to be used during the connection and the disconnection process.
- Storage of disposables: Two wardrobes with wire baskets are ideal for storage of concentrates, needles, tubings, dialysis filters, and other disposables that are used during the dialysis treatment. Some people just stack the boxes in a dry area.
- Water Treatment: Dialysis always carries a risk of water leaks. If possible it should be installed in a room with a floor drain. Water leakage detectors are an option.
- Phone: Always instruct the patient to have a phone close by for emergency calls.
- Dialysis machine: Avoid placing the machine on unprotected regular carpet as there is often some leaking water or saline around the machine.
- Waste: A waste bin will be needed for consumables after use. A secured box is required for needles.
4.6.3 Checklist for appropriate home environment
A home assessment is done by a team that usually includes a nurse and a technician. The timing of the assessment may vary according to the dialysis units’ policy: at the time of dialysis modality selection, before or during the training process. The checklist gives some ideas of what should be checked.
| Checklist | Yes | No | Comments |
|---|---|---|---|
| Electric supply available | |||
| Electrician review for safety requirements | |||
| Clean water supply available | |||
| Water quality-standard tests complete | |||
| Water pressure adequate | |||
| Machine preference determined | |||
| Room for dialysis determined | |||
| Space for storage available and clean | |||
| Waste disposal available | |||
| Drainage accessible (Need plumbing assessment or changes) | |||
| Option for reject water use (desirable) | |||
| Appropriate lighting | |||
| Appropriate chair/bed | |||
| Clean environment | |||
| Pet free treatment room | |||
| Access to land line or cellular telephone network |
4.7 Maintenance of HHD
4.7.1 Home visits
The first three months after initiation of HHD are the most crucial, and affect whether the patient will successfully continue this treatment modality. Weekly home visits during the initiation period may be very useful, as well as having the patient call the nurse both before and after completing each dialysis procedure, and having on-call support 24/746. Then home visits may be provided as necessary, most of the units provide on average 3 home visits per year.
Detail on home visits can be found in the chapter on support.
4.7.2 Logistics
Supply delivery: Supply delivery to patient’s home most of the time is done by the company that is responsible for dialysis machine equipment. Sometimes a common carrier may be used and supplies will be brought to the door or into the home. The frequency of supply depends of the home storage size, frequency of the treatments and the distance from the warehouse. In some countries deliveries at home may be under the responsibility of a pharmacist to check matching with prescription then delivery route may require a specific organisation.
Waste disposal: HHD produces a large amount of waste products. Most of the waste is considered as biohazardous waste, and requires appropriate storage and pick-up. All sharps waste should be collected in special containers. HHD education programme should include explanations regarding local regulations for biohazard waste disposal. Each country or council will have its own regulations regarding waste management. It is the responsibility of the dialysis unit to know the local regulations and share these with the patient.
(See the Chapter 11 on environment for some handy hints about waste disposal).
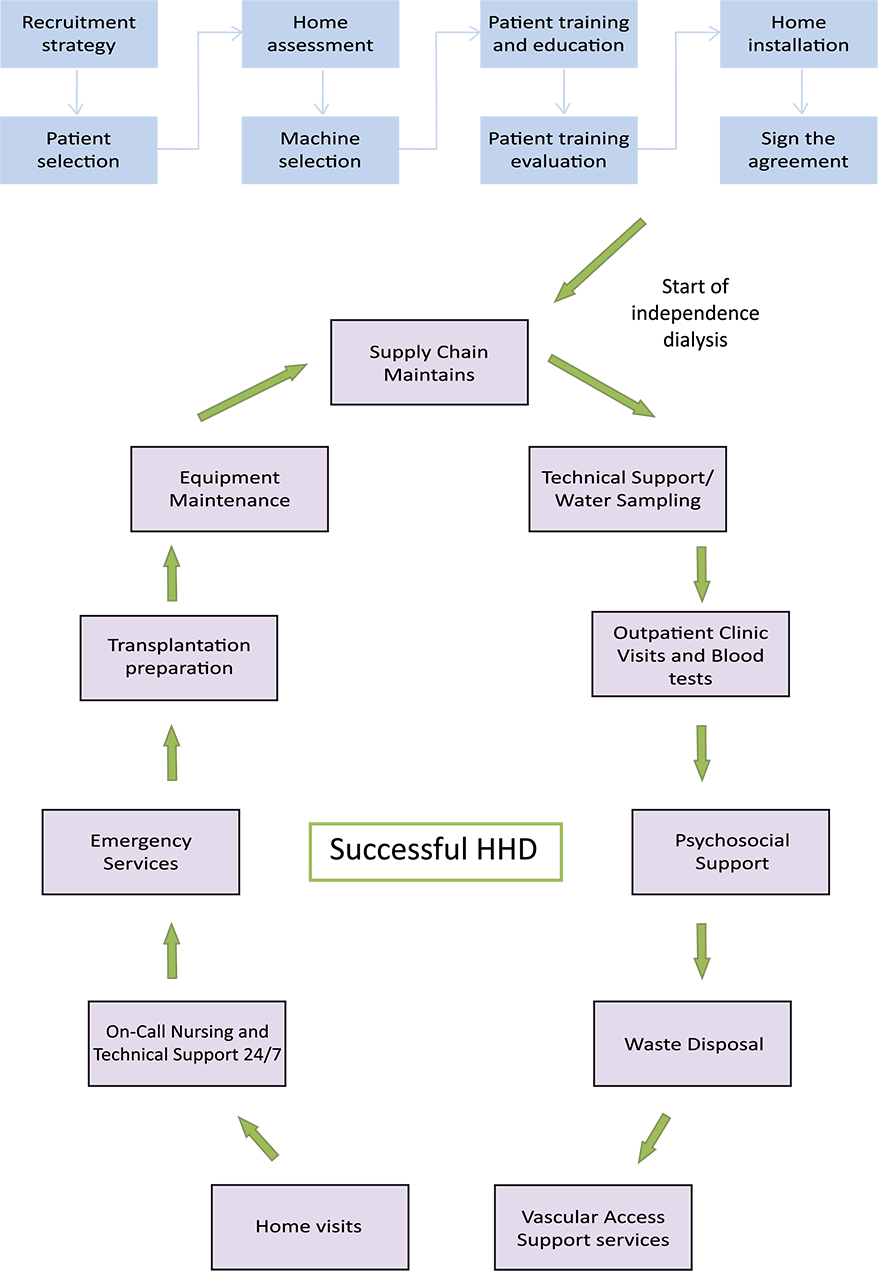
4.8 Summary of Process of Home HD
After completing a preparation process that includes installation, patient education and training, the patient is ready to go home for dialysis. Patients’ expectations regarding home treatment should be reviewed and communication with a dialysis unit nurse and physician should be a part of the educational process.
An agreement with the patient regarding the HHD process and roles and responsibilities may be used in some units.
All stages of implementation of HHD are shown in the graphic in paragraph 4.7.1.
Summary
In this chapter we have discussed the basic issues for successful HHD. This treatment modality is appropriate for many dialysis patients. There are various therapy options for HHD. Patient’s health status, lifestyle preferences, place of living and treatment goals play an important role during the planning process of HHD treatment. The Dosing calculator is a very useful tool that can help to plan each treatment. All types of VA can be used for HHD, however it is essential that it works properly and the patient receives appropriate anticoagulation treatment during dialysis. Home installation, required equipment, environmental and logistic processes are important challenges for successful implementation of HHD. Home visits by the nephrology team and professional intervention for home adaptation may be needed.
Learning Activity
- What patient populations can benefit from HHD?
- What are the options for prescriptions for HHD?
- What is the Dosing Calculator and what can it be used for?
- What differences exist between anticoagulation of in-center haemodialysis versus home haemodialysis?
- What types of vascular access can be used for HHD?
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org