







Nicola Pacy
RGN. Home Haemodialysis Manager, Wessex Kidney Centre
Queen Alexandra Hospital, Portsmouth, UK
nicola.pacy@porthosp.nhs.uk
8.0 Ongoing Support
Learning Outcomes
- To understand the support required for home dialysis patients and carers
- To understand how to provide the support for patients and careers
- To understand staff and patient responsibilities that ensures adequate and safe governance
Introduction
Support of patients at home is integral to the success and maintenance of a home programme1. However, to make certain a home programme is successful we need to ensure that we not only give support to the patients but also their partners, as the impact of home therapies affects everyone who lives in the home1. In this chapter we will take you through the support mechanisms that should be put into place to provide a successful support network for all involved2.
8.1 Dialysis adequacy and well-being
8.1.1 Check ups and general support
All patients at home should be offered regular contact from a member of the home team which can be a home visit, attending a nurse led clinic or telephone and e-mail support. Frequency will depend on the patient and local policy but a minimum of monthly check-ups are common. Consultant clinics are usually attended quarterly3.
8.1.2 Visits to center
If there are robust processes in place to support patients at home the need for visits to the main unit should be negated. A quarterly review by the nephrologist will still be required although this can be done at a local satellite unit if possible therefore reducing travel time. A nurse led clinic can be beneficial as it offers additional support to those patients that need it and can incorporate vascular access, dietetics, anaemia management and dialysis adequacy reviews.
8.1.3 Blood sampling
Patients are usually responsible for taking their own monthly blood tests and sending to pathology via General Practitioner/satellite dialysis units or the home nurse. Some centers advise patients to attend their local pathology center or clinic so that bloods can be sent in a timely fashion. Most units will follow the unit policy for in center HD patients, typically this will be:
- Pre dialysis renal biochemical profile and post urea (for adequacy calculation) monthly.
- Full blood count monthly.
- Hepatitis B, C and PTH 3-6 monthly.
- Iron studies as requested (often quarterly).
- Patients may also be responsible for taking their transplant bloods.
All blood results should be reviewed by a member of the home team or consultant and acted on accordingly. Prescription changes can then be made as needed.
8.2 Patient empowerment
8.2.1 Expert patient and carer
Patients on a home therapy tend to become an expert patient enabling them more control over their health and treatment options. Involved carers often have the same status. Becoming an expert patient is empowering for patients with chronic conditions and with this comes increased engagement and responsibilities4. The patient is responsible for adhering to the prescription and carrying out their therapy as they have been trained. Most units will sign them off as competent to do this. Patients should also report any problems or issues to the home team and in return the home team are responsible for providing feedback or support to solve the problem.
8.2.2 Safety
It is the responsibility of the training nurse to ensure that the patient is competent to perform the home therapy in a safe and supported environment. Training materials will be used to help guide and teach patients about their therapy. The trainer must ascertain the individuals level of knowledge and understanding and gaps in learning, e.g. due to dyslexia, and ensure that the appropriate support tools are available5. Learning checklists may be helpful. An informed and educated patient can actively participate in his or her own treatment, improves outcomes and helps to identify errors before they occur6,12.
8.2.3 Community support
It is the joint responsibility of both the home team and the patients to make sure that community services have been informed that home dialysis will be carried out. Letters may need to be supplied to:
- Clinical waste services
- General Practitioners
- Utility providers (electricity/gas/water)
8.3 Procedural support
8.3.1 Machine troubleshooting
Basic trouble shooting will be taught during training. The level of support given by the company in troubleshooting will depend on the equipment chosen for the home therapy. Some centers have dedicated renal technicians who are available to support the patients at home. Some companies will provide a dedicated 24/7 helpline that the patients can access and if necessary a new machine can be sent to the patients’ home within 24 hours. With Frequent Home Haemodialysis (FHHD), in case of unsolved technical issue, it may be possible to rinse back the blood and repeat a session the next day, after the problem is solved.
8.3.2 On call
Some centers will offer a 24 hour on-call service which will offer advice and support for any clinical or technical problems that are encountered. Separate on call may be provided for nursing (clinical) and technical issues. It is important the patient is clear on who to contact, how and when. It is also important that they know that issues that are not dialysis related are managed by their usual community health professionals.
8.3.3 Managing machine alarms
All patients must be confident in the technical aspects of their care and how to rectify and act upon machine alarms competently. This should be incorporated into their initial training package. Simple trouble shooting guides, either paper or online will simplify the process, especially when a rare machine alarm occurs.
8.3.4. Remote monitoring and technology
The use of technology is becoming more popular with the use of specially designed Apps that can record dialysis sessions and problems so that center staff are able to access the data in real time and act upon it. Some centers use Skype to communicate with their patients and having access to an e-mail address is helpful9.
Patients in the UK are able to monitor their own bloods with the use of Renal Patient View to manage blood results and if your country has a similar system patients should be encouraged to access this.
8.4 Maintaining competency
8.4.1 Competencies
All patients should be provided with training materials, competency documentation and troubleshooting guides. All competencies should be signed by training nurse, patient and or care partner.
As part of the home visits competencies should be reassessed and retraining given where appropriate. Patients should be made aware that competencies will be reviewed regularly.
8.4.2 Re-training
On routine monthly visits the patients’ hand-washing technique can be reassessed. The vascular access should also be checked for signs of infection.
If patients have been hospitalised for a long period of time and may have lost either physical or mental capacity, then retraining should be offered, either in their own homes or within the home training area. Additionally, a visit from a member of the home team should be arranged for the first treatment following discharge to ensure the patient is competent in their home environment and the machine is still functioning properly.
See training chapter for more information on competencies.
8.5 Vascular Access
8.5.1 Vascular access monitoring
Pre-emptive surveillance programme for vascular access should be carried out on a regular basis as this may increase patency rates and decrease the incidence of complications7. Vascular access monitoring for flows and potential stenosis should be part of any HD program but will vary by center. For patients on HHD, vascular access monitoring should be carried out as close to usual center policy as possible.
During training patients are taught to recognise and identify the signs of infection, failing access indicators, for example raised venous pressures, prolonged bleeding times and difficulty with cannulation. Trend monitoring of these signs and review of these at check-up are useful in detecting issues with vascular access.
If the equipment is available transonic readings can be performed as part of the monthly home visit. Transonic readings should then be routinely submitted to the appropriate access specialist for review.
8.5.2 Vascular access specialist
To preserve the function of all types of vascular access the involvement of the vascular team or a specialist fulfilling this role is useful. All patients should know who to contact if there are vascular access concerns. It is often the responsibility of the designated vascular access specialist to arrange fistula-grams and any interventional procedures that are required.
The vascular access specialist can also play a role in developing changes in policies and guidelines in relation to infection control and changes in procedures for vascular access.
8.6 Home Visits
8.6.1 Safety at home visits
Prior to commencing training an initial home visit should be performed to assess the suitability of the home. A risk assessment should be carried out at this time and annually thereafter to ensure the safety of the patient, and also for the staff who will be required to visit the patients home. See the risk chapter for more detail.
8.6.2 Frequency of home visits
It has been the experience of the author that following training, home visits should be scheduled weekly for a period of four weeks and then monthly. A risk assessment rating tool should be used to determine if the patient requires extra support, in the form of a phone consultation or additional visits. A risk assessment tool can be found in the risk chapter.
8.6.3 Process of home visits
Home visits should be structured and the use of a checklist is beneficial to make sure that no aspects of care are missed. The home environment should be assessed and a check of the machine carried out from an infection prevention perspective. It is equally important to involve care partners in the home visit to identify any carer burden that may be developing and assess if respite care is required. If signs of dyscopia are evident (such as a neglected house or personal hygiene) it is important to follow up these signs, or just ask the patient what is the biggest concern for you right now?
8.6.4. Home Visit Checklist
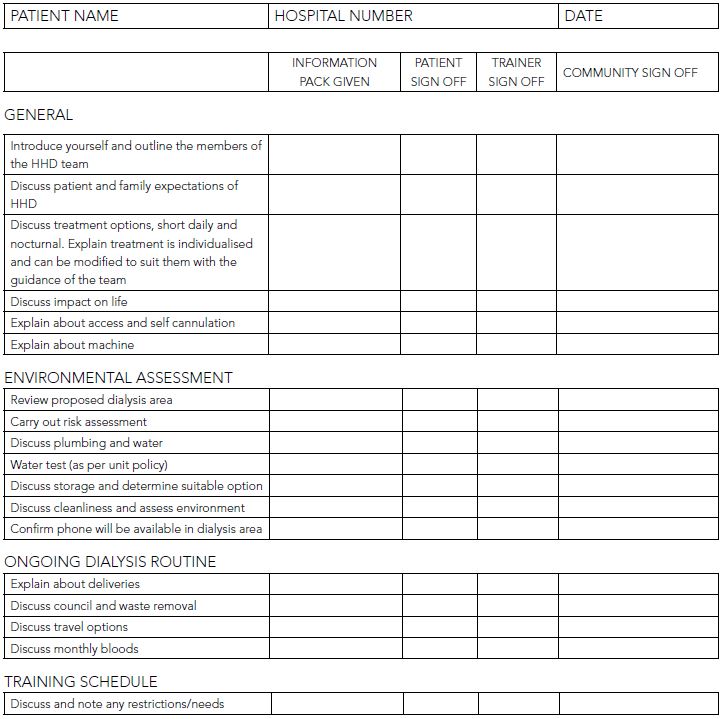
To maintain structure it is important to use a checklist for any home visit. A sample checklist for a pre-home dialysis visit is provided in Appendix 1. The home visit should be tailored to each patients’ requirements, looking at their physical, social and psychological wellbeing.
Pre-home visit
It is ideal to conduct a home visit prior to first clinic appointment for those patients who have expressed an interest in HHD. Prior to visit contact patient to arrange convenient time for visit.
Document visit on paper or computer system.
Appendix 1 – Checklist for Pre-home dialysis visit
8.6.5 Water Samples
Water and/or dialysate testing for bacteria, endotoxin and chemistry should be performed according to each individual center guidelines and policies for HHD generally. Adaptations may need to be made to in-center protocols but not compromise patient safety. However, the NxStage therapy handbook does not recommend the need for water testing when dialysis is being performed on a NxStage machine.
8.7 Quality of Life
8.7.1 Quality of life measurement tools
There are a number of quality of life tools available, it is useful to ask the patients to complete one at the beginning of the training and then annually. This helps to obtain general information about the patients physical and psychological well-being at the onset of transitioning home and the benefits that they may identify as a result of performing a home therapy7. It also allows identification of a patient who is deteriorating.
For example the Kidney Disease Quality of Life (KDQol) SF-36 questionnaires have become widely used10. It is apparent that dialysis patients have higher scores on the emotional components of these assessments than controls, indicating, perhaps not surprisingly, that emotional difficulties are present in dialysis patients13.
8.7.2 Psychological support
If patients are showing signs that they could be depressed or they voice experiencing psychological issues, referrals should be made to the appropriate agencies. Depending on local availability this could include counselling services, social workers and psychologists.
8.7.3 Support groups
Local support groups may be beneficial for both social and financial support. Charitable organizations may be able to offer grants to help with financial difficulties, the British Kidney Patients Association being one. If there are no organisations offering a support group local to your unit you could facilitate a patient and carer support group for your patients. It can be as simple as a coffee morning.
Many countries have specific carer support agencies who can offer support to carers.
8.7.4 Respite care
If possible there should be the option to offer respite for patients and carers if the need arises. This can be by offering dialysis at the training center, the local dialysis unit or maybe a nurse to provide some dialysis support at home if that service is available. Many countries have private nursing agencies that may be able to help if the patient can pay.
8.7.5 Financial support
Financial stress is common for families using dialysis and many people on dialysis have reduced family income11. However, the flexibility of HHD should facilitate return to work, potentially reducing financial stress. HHD patients should be asked if they have any financial stress and it is important that the home dialysis team or the social worker are aware of benefits or reimbursements that local patients can claim and how to refer to these services.
8.8 Nutrition
8.8.1 Nutritional status
Malnutrition is a predictor of poor outcomes. There are many ways to measure nutritional status and details are provided in the nutrition Chapter 10. For example, the use of a Malnutrition Universal Screening Tool (M.U.S.T) is helpful in determining which patients require extra dietetic input. Utilising this tool also includes management guidelines which can be used to develop a care plan to ensure avoidance of malnutrition at home8.
Most units that offer the service encourage regular appointments with a dietitian to individualize diet and fluid intake. More general detail about nutrition is provided in the Chapter 10. Litterature also showed that patients on FHHD or Nocturnal HD (NHD) may experience improved appetite and fewer dietary restrictions14,15,16,17,18,19,20.
Summary
Good support at home can extend the time someone stays on HHD and their quality of life on HHD. Each unit must have a structured system to provide support with consideration to individual needs.
Learning Activity
- How often should patients have contact with the home dialysis nursing team?
- What are the patient’s responsibilities?
- How can you support a patient to achieve the best quality of life they can?
- What assessments should occur on a home visit?
- How can carers be assessed and supported?
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org



