






Gunnar Malmström
Electrical Engineer. President for MTFD, Swedish Association for Dialysis Technologists
Danderyds Hospital Medical Technical Department, Stockholm, Sweden

Sophie Halldin
RN, Renal Unit in Haemodialysis Department, Danderyds Sjukhus AB
Stockholm, Sweden
elsahalldin@yahoo.se

Monica Edström
RN, Renal unit in Home Haemodialysis Department at Danderyds Sjukhus AB,
Stockholm, Sweden

Marie-Louise Bodin
RN, Renal unit in Home Haemodialysis Department at Danderyds Sjukhus AB
Stockholm, Sweden
9.0 Safety and Risk Management
Learning Outcomes
- To understand the right framework that can improve HHD safety
- To understand the Quality Assurance loop
- To understand some useful risk assessment processes
- To be aware of potential HHD complications and related specific prevention
- To gain an understanding of Venous Needle Dislodgement
Introduction
Home Haemodialysis today, is generally very safe. This may be because patients are highly selected prior to initiating home therapy and because they initially spend many weeks learning the technical aspect of self-managing the dialysis procedure1.
There have also been advances in machine technology that have reduced technical complications and longer and more frequent treatments have reduced the risk of hypotension and cardiovascular instability2.
Traditional HD patient safety focuses on the care provided by health care professionals. Safety in HHD also involves the patient partnership with their care partner and health care professionals. Patient safety during HHD must also include a proactive stance to minimize patient injury in the event that an error does occur3.
One big important part of safety is to communicate risks to patients. The conversation with patients aims to balance the benefits of HHD with the risks and increased burden of independent HHD. While the risk for HHD will never be zero, patients are reminded that HHD is very safe and that great care has been taken to design resources, policies, and procedures specifically aimed to minimize risks3.
9.1 Quality Assurance
It is relevant to apply a framework of quality assurance to a HHD program so that adverse events can be avoided. Overall event rates for technical complications in HHD are low in most cohorts, the potential for these events to be fatal emphasizes the need for quality assurance by event reporting, and quality improvement1.
Experienced HHD programs have well established frameworks to minimize the impact for potentially serious adverse events and, if they do occur, to manage them effectively. New HHD programs will benefit from these lessons and must instill a culture of safety – without inciting alarm or undermining assurances – that HHD is a generally safe therapy. A blame free culture is necessary so that safety can be prioritized3.
The treatment environment, the home setting, should be designed with both safety and comfort in mind (See Chapter 4, Basics of HHD)3.
9.1.1 Education
Serious adverse events during HHD are rare and this is due mainly to the use of educating patients in safety procedures. Training is the key element in preventing serious adverse events3.
A successful HHD training program must focus on patient safety. Considerable time should be devoted to troubleshooting machine alarms and responding to emergency situations, including power outage and accidental disconnection1. Strict routines to prevent serious hemorrhage from needle dislodgment and enable an aseptic cannulation technique are two big focus areas. In addition, vigilance in relation to machine maintenance procedures and attention to water quality are key skills that patients must acquire for optimal outcomes2.
Communication plays a key role in the avoidance of error. Training staff should provide clear messages and communication around safe practices and clarify the responsibility between patients and care partners around procedures/protocols, while emphasizing the final objective for training: technically excellent dialysis performed in the home, without compromise to safety3.
However, it is important to be aware that a fear of catastrophic events is a patient-perceived barrier to adoption of HHD4. Education about event reporting is also an important undertaking. When an adverse event happens, appropriate identification of the cause and retraining should take place.
Education of care partner – The same attention is required for training and maintaining competence of care partners as it is for the patients themselves3.
9.1.2 Quality assurance loop
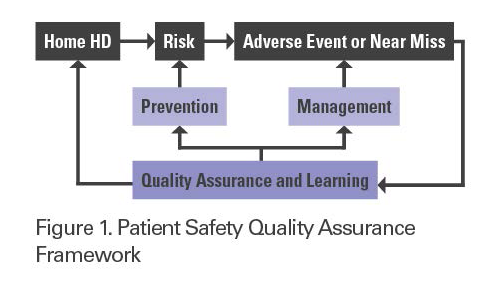
Central to any safety framework is an interactive quality assurance loop designed to prevent or minimize the occurrence or recurrence of an adverse event for an individual patient, and for other patients within the same program. The three steps in developing a quality assurance process:
- Identification of the key risks.
- Establishment of robust standard operating procedures for HHD.
- Documentation of process measures related to outcomes and safety. Process measures should include a key performance indicator for near misses. In addition, regular near miss conferences should be held among the clinical staff within the training unit. Where possible, lessons learned from near misses and serious adverse events should be incorporated into the HHD patient teaching curriculum. Existing patients within the program should be made aware of changes in policies and procedures during follow-up visits or by use of periodic communication from the program3.
The principles of a quality assurance loop include early management when risk is identified and interventions for future prevention when an adverse event or near miss occurs (Diagram 1).
Diagram 1. A Quality Assurance loop – patient safety quality assurance framework
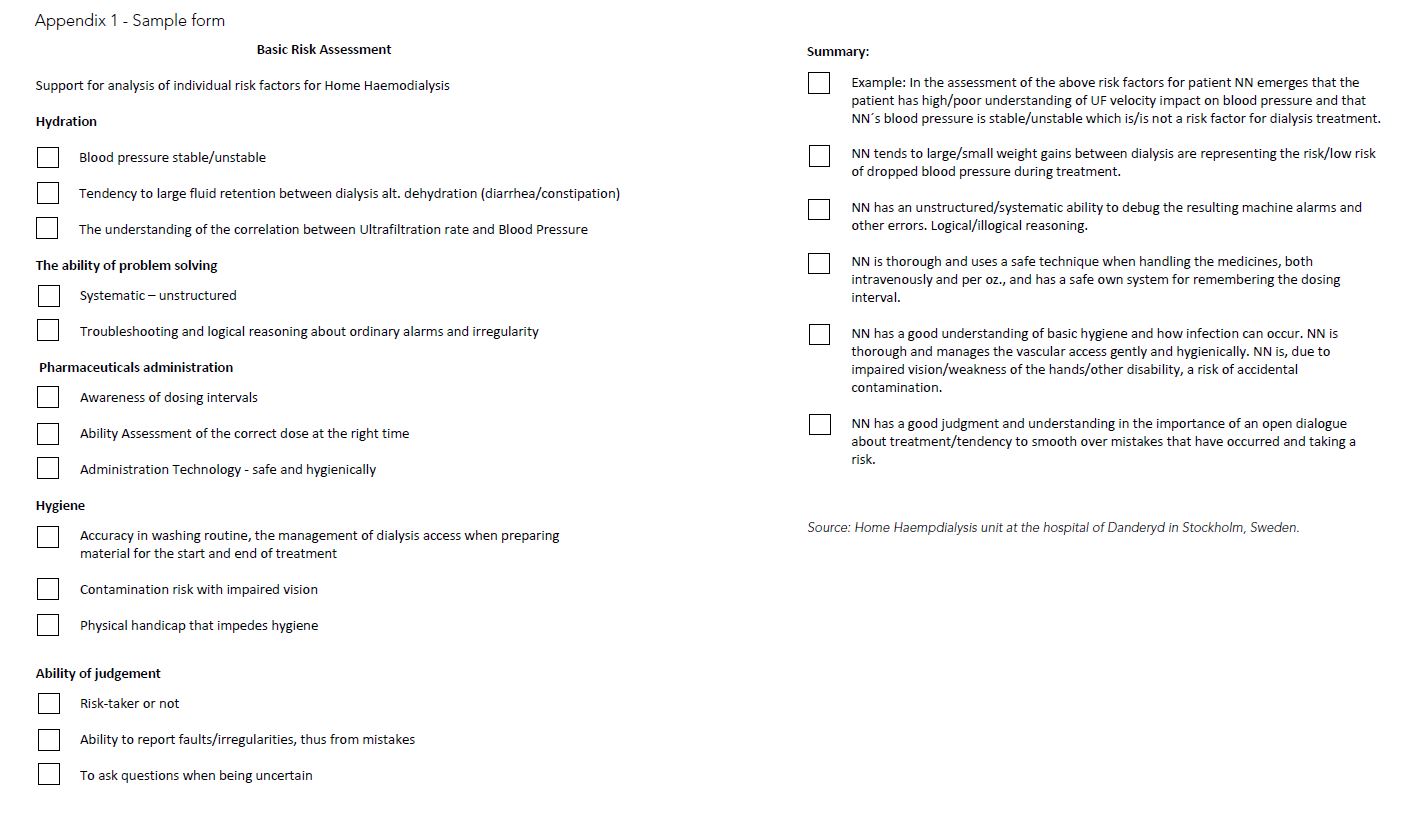
9.1.3 Patient risk assessment
Patients using HHD have gone through extensive training and many units ask them to sign a liability form and/or provide certification of competency with HHD. To ensure that the patient maintains their skills and does not take unnecessary risks, an evaluation of their risk should be performed regularly. Below is a suggestion of how that form could be designed.
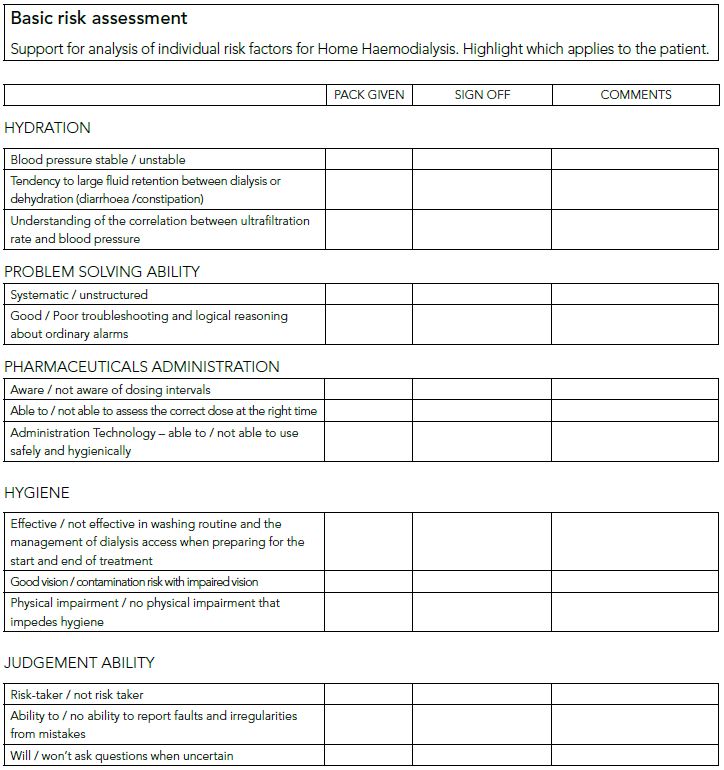
Example assessment of Mr. X:
- In the assessment of the above risk factors for Mr. X it emerges that he has poor understanding of UF velocity impact on blood pressure and that Mr. X´s blood pressure is unstable (high risk of low blood pressure).
- Mr. X tends to large weight gains between dialysis which contributes to a high risk of dropped blood pressure during treatment (high risk of low blood pressure).
- Mr. X has a systematic ability to manage the resulting machine alarms and other error with logical reasoning (low risk of machine issues).
- Mr. X is thorough and uses a safe technique when managing pharmaceuticals, both intravenously and orally, and has a safe system for remembering the dosing interval (low risk of drug errors).
- Mr. X has a good understanding of basic hygiene and how infection can occur. Mr. X is thorough and manages the vascular access gently and hygienically. Mr. X has impaired vision and weakness of the hands (high risk of accidental contamination but low risk of infection)
- Mr. X has a good judgment and understanding of the importance of an open dialogue about treatment but has a tendency to smooth over mistakes that have occurred (medium risk of errors).
It is important that strategies are put in place to minimize areas where Mr. X is at medium or high risk. These may be step-by-step procedures or more training.
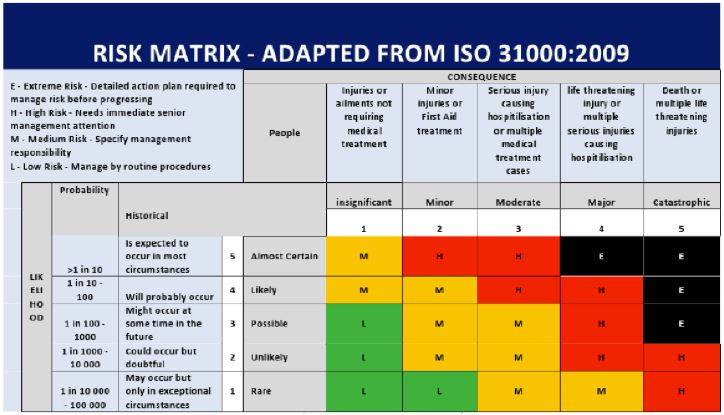
9.1.4. Risk assessment matrix
Risk management programs and adverse events systems should utilise a grid that determines the risk of an event occurring against the potential outcomes. This is useful to determine the level of resourcing to be used to prevent a risk. If the risk of an event occurring is high and the outcomes catastrophic then that risk must be addressed. Also, if the risk of an event is high even if the consequences are generally low measure must be put into place i.e. hypotension on dialysis.
Diagram 2 shows an example of a risk matrix6.
9.2 Risk management process
When or if an incident occurs, it is most important that the patient has been trained how to manage this circumstance. One example is a major issue that means dialysis cannot safely continue. The patient is taught to discontinue dialysis and can be provided with a visual reminder “algorithm“. All patients can be given a preventive emergency kit with the algorithm and emergency equipment for disconnection directly positioned near their HHD machine.
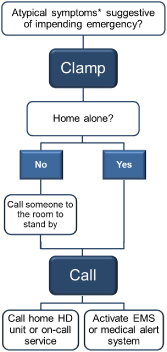
9.2.1 Emergency algorithm
Significant (potentially life-threatening) adverse dialysis event i.e. major equipment failure, severe hypotension or vascular access bleed requires immediate action and the patient should have a quick reminder available.
A sample “Clamp and Call” emergency management algorithm is provided in Diagram 3.
9.2.2 Contact accessibility – management of adverse events
Clinical and technical assistance for patients and their care partners should be easily accessible 24 hours/day. Patients should be clear about how to contact emergency medical services and know the location and contact details for their nearest hospital emergency department (See chapter on Basics in HHD)3.
9.2.3 Follow-up after a serious adverse event
Serious adverse events are those that involve hospitalisation or death. Every hospital should have policy and procedure for adverse events, and these apply to HHD programs. Below is an example of steps to consider after a serious adverse event3:
The root cause needs to be determined.
- If consequences are severe consider if the machine and consumables should be impounded ‘as-is ‘from the patient’s home, without being stripped or cleaned, and stored for examination in the home haemodialysis training unit.
- All documentation resulting from the treatment should be submitted. Copies should be made and the originals stored securely to prevent inadvertent loss of key paperwork.
- The sequence of events and context of the event should be ascertained as clearly as possible from those present at the scene and through the liberal use of photography of scene and machine.
- Depending on the nature of the event, the machine should be examined for any stored information (e.g., blood pressure measures, alarms, alarm overrides).
- Depending on the nature of the event, haemodialysis technical staff (ideally from an external, independent home HD training unit) should ensure that the machine meets standard operational checks.
- There should be immediate communication of the potential for the specific error in question to the HHD training staff and existing home haemodialysis patients, as necessary.
- Depending on the nature and severity of the event, there might be an external review of the HHD training program and its resources by the quality improvement team of the parent hospital or another home haemodialysis training unit with more experience. The review may involve root cause analysis or failure mode and effects analysis (i.e., techniques for delineating error that are usually beyond the capabilities of clinical staff).
- Depending on the nature of the event, there might be communication with the manufacturer of the dialysis machinery to ascertain whether the event has occurred previously, and whether a technical solution is available to prevent similar events.
- Depending on the nature of the event, consideration might be given to publication in an open-source medical journal, as this is likely the best method of communicating widely with clinicians.
- Depending on the nature of the event, consideration might be given to communication of the event on a reputable Web-based patient discussion forum, in conjunction with a patient advocacy group.
- It is recommended that each unit keep a registry of serious adverse events, and communicate these events and near misses to other providers in their region to share experience.
9.2.4 Follow-up after a minor/moderate adverse event
Minor or moderate adverse events include significant hypotensive episodes that are managed without needing hospitalisation, needle dislodgement with minor blood loss and equipment failure.
All adverse events should be logged on a form or in a central database. This database should be reviewed regularly to track trends and patterns in frequency of events. The form should include;
- Details of the event including outcome.
- Potential cause (root cause analysis).
- Actions taken to prevent future occurrence.
Regular policy and procedure review should take place if an adverse event is increasing in frequency. Changes to practice must be communicated to all patients.
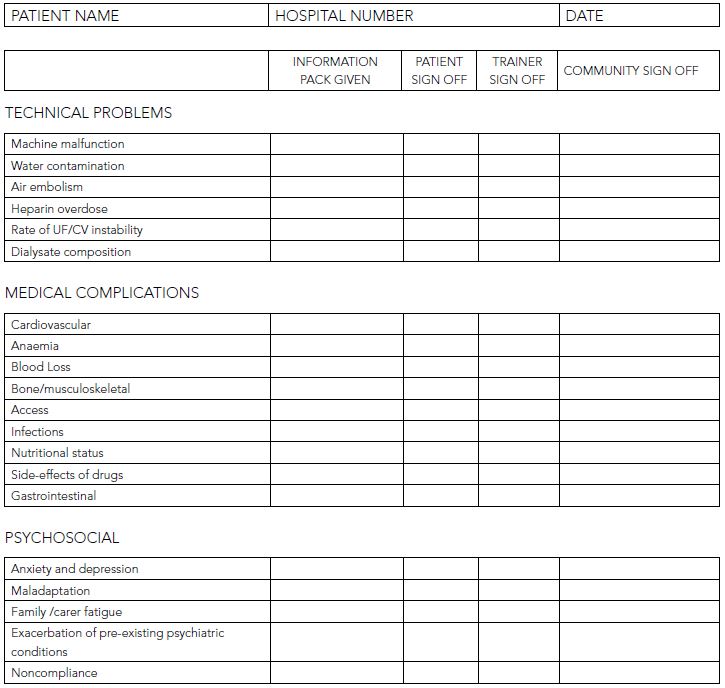
9.3 Potential risks/complications of Home Haemodialysis
Performing dialysis in a home setting can generate the same complications as in-centre haemodialysis (ICHD). In addition, there are complications that occur in the home setting because of the absence of professional assistance in machine and water maintenance and in trouble-shooting in the event of problems2.
There should be strategies and policy and procedures in place to manage and prevent all of these risks and complications (potential adverse events).
Complications can be divided into three areas:
9.3.1 Technical safety
Home dialysis machine safety requirements do not differ from centre based machines and they must meet international and national safety standards in order to reduce risk. The safety mechanisms include:
- Pre-dialysis safety check.
- Recommended priming procedures (include ways to minimize infection risks).
- Dialysate conductivity alarms.
- Ultrafiltration monitoring.
- Blood flow pressure alarms.
Summary of potential risks:
- Blood leak alarms.
- Safety limits that can be pre-determined.
- Air detector mechanisms (to prevent air embolism).
- Disinfection procedures to ensure good water quality.
- Safety cutout mechanisms for electrical risks.
The patient must be taught to follow procedures that maintain this safety and also how to contact technical support if alarms occur related to machine functioning.
Regular servicing of machines and water treatment equipment as per manufacturers recommendations is critical. Servicing can be done at home or by machine swaps to the technical department.
Regular water testing is also a key part of technical safety. National guidelines must be adhered to.
Finally, electricity, water and patients do not mix well. There must be mechanisms in place to prevent accidental electrocution by either macro-shock or micro-shock. Residual current leakage detectors with a power cut out at 10mAmps is recommended, either directly linked to the dialysis electricity provision or the household. Every country will have its own guidelines on medical equipment power supply and each dialysis unit must develop relevant policies.
9.3.2 Medical complications
The medical complications can be similar or can arise from different causes compared to ICHD;
- With Frequent Home Haemodialysis (FHHD), there is a higher risk of problem incidence on the vascular access such as infections and access rupture.
- Higher rates of specific non-access-related infections (e.g. pneumonia and sepsis) were observed in HHD patients compared to access-related infections5.
- Cardiovascular problems such as hypotensive crisis or overload of fluids can occur but are usually seen less frequently than in ICHD.
- Malnutrition can occur due to “overdialysis” with loss of nutrients (including water-soluble vitamins)1,2.
- Side-effects of drugs and gastrointestinal complications can occur1,2.
Regular check-ups, blood tests and technique checks can reduce the risk of medical complications.
9.3.3 Psychosocial
All patients on dialysis have a high risk of psychosocial complications including; anxiety and depression, maladaptation, family /carer fatigue, exacerbation of pre-existing psychiatric conditions and noncompliance2. Regular assessment and communication will detect if a patient has any of these psychosocial complications.
Patient and caregiver burden – FHHD necessarily increases the number of days per week that are accompanied by dialysis treatment. This may increase the burden of dialysis on patients and care partners and lead to reversion to ICHD. Choosing the dialysis routine in close collaboration with the patient is important to minimize this risk.
9.3.4 Life-threatening adverse events
All of the above categories have complications that are potentially life-threatening adverse events. The three most common causes of life-threatening adverse events in HHD are:
- Blood loss – bleeding from the circuit (due to poor connections between tubing and access or dialysers) or bleeding from access dislodgement.
- Human error – patients failed to follow prescribed procedures; e.g. ignoring machine alarms or neglecting to appropriately use wetness detectors (see VND section). This underscores the importance of human error and the observation that patients will find a multitude of unpredictable ways to modify their dialysis that contravene standard operating procedures specifically designed to reduce the risk of accidents.
- Lack of patient awareness – that even small seemingly insignificant change in a procedure may lead to serious consequences1,3.
9.3.5 Venous Needle Dislodgement (VND)
Patients and carers should be aware of VND and the consequences7. Two main factors must be taken into consideration to avoid any risk of VND:
Step 1 – Factors affecting how well secured the needles are. These risk factors will make it more likely that a VND incident will occur, either due to a higher risk of tugging on the lines connected to the needles, or to a higher risk of the taping of the needles not being able to hold the needles in place.
- Patients prone to erratic or restless behavior, e.g. intradialytic hypotension, cramping.
- Patients with a history of VND.
- Patients with oozing around venous needle.
- Patients who have a high degree of sweating around the access site.
Step 2 – Factors affecting the ability of patient/carers for a proper monitoring. These risk factors will make it less likely that in the event of a VND event, the carer or the patient will observe the incident and either take suitable remedial action or raise the alarm for somebody else to act.
- Poor lighting in the room.
- Patients covering the access during dialysis.
- Dialyzing in isolation rooms.
- Self- care or minimal care support.
- Tendency to sleep during dialysis.
- Temperature/fever.
- Reduced sensitivity.
The patient who opts for HHD should have appropriate training on procedures for taping needles and bloodlines to be followed at every dialysis treatment:
- An area around the vascular access large enough for taping should be cleaned and air dried before cannulation.
- Bloodlines should be looped loosely to allow movement of the patient and to prevent bloodlines pulling on the needles.
- If it is necessary to reposition a needle, lower the blood flow to 150 ml/min and replace all taping.
- All patients should be assessed for level of risk of VND and, if appropriate, an alarm device intended for monitoring venous needle dislodgement used.
- Vascular access and needles should be visible at all times during haemodialysis.
- When the venous pressure alarm is activated, the vascular access and fixation of needles and bloodlines should always be inspected prior to resetting the alarm limits.
- Patients and carers should be aware that the venous pressure monitoring system of the dialysis machine will often fail to detect VND.
- Additional protection can be provided by devices intended to detect blood loss to the environment.
Staff and patients can also access the Venous Needle Dislodgement App developed by the EDTNA/ERCA8 (Temporarily unavailable at this moment).

Summary
Safety and risk management is a critical part of any HHD program. This chapter has highlighted some of the key risks. It is important that all units follow hospital policy and procedure to develop risk management programs.
Learning Activity
- What are the key elements in preventing serious adverse events?
- What are the key steps in developing a quality assurance process?
- What is VND?
- What is the “Clamp and Call” algorithm about?
- What are the three most common causes of life-threatening adverse events in HHD?
Appendix 1 – Sample form
Basic Risk Assessment.
Click on the image to open or download the form for use on your computer or mobile device.
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org



