







Pedro Miguel Reinas André Pereira Baptista
RN, H. U. La Princesa
Madrid, Spain
pedroreinas@gmail.com
11.0 Environmental Home Haemodialysis
Learning Outcomes
- To understand how much dialysis can contributes to the carbon footprint worldwide
- To identify the key dialysis causes of the carbon footprint
- To understand the differences in production of carbon between standard haemodialysis and HHD
- To identify opportunities to reduce the carbon footprint
Introduction
In this chapter we will address the green side of home dialysis versus traditional haemodialysis in a hospital.
Green dialysis is important because we know that patients diagnosed with end-stage kidney disease are increasing. Prolonged life expectancy and increasing incidence related to diabetes contribute to this increase. It is predicted that in 2020 there will be 3,500,000 patients worldwide in renal replacement therapy1.
To accompany this rapid advance in medicine, its diagnostics and its treatments, there is high use of energy, water, and raw materials such as plastics, which also leads to a higher production of waste.
This chapter has the purpose of raising awareness to avoid sparing resources. It discusses resources such as water; electricity; logistics; and waste. Evidence will support this information to facilitate informed decision making regarding green dialysis.
This chapter is just a brief overview and a website entitled Green Dialysis provides more details on this topic2. Some countries also have organisations targeting green dialysis. Look for your country on social medias and the internet to see if there are any groups available in your area.
11.1 Basics of environmental HHD
11.1.1 Kyoto Protocol
The Kyoto Protocol on Climate Change is an international agreement that aims to reduce the emissions of six greenhouse gases that cause global warming: carbon dioxide (CO2), methane gas (CH4), nitrous oxide (N2O), and 3 fluorinated industrial gases: perfluorocarbon hydrofluorocarbons (HFCs) and sulfur hexafluoride (SF)6.
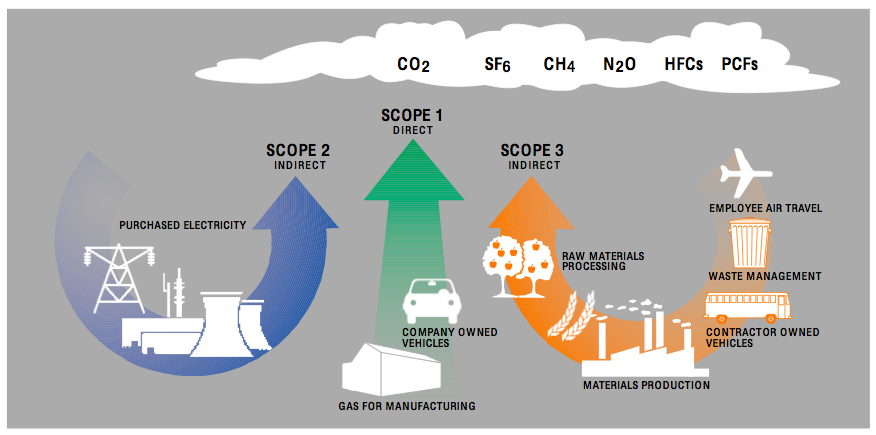
Source: GHG Protocol
This translates into the Carbon Footprint; “The measure of the impact our activities have on the environment, especially on climate change”, that is, the quantification of direct and indirect emissions of greenhouse gases, such as those described above. These are released to the atmosphere as a consequence of the activity of a company, the life cycle of a product, the organization of an event or the activity of a person.
The purpose of this protocol is to contribute to a healthier environment, and support the ability of countries to control the carbon footprint, avoiding its increase with basic measures in our day to day activity.
11.1.2 Measuring carbon footprint
For green dialysis it is important to understand the carbon footprint of each type of haemodialysis:
- Haemodialysis in a hospital;
- Standard Home Haemodialysis.
- Home Haemodialysis with NxStage System3.
A key UK report included: energy used, dislocations of both, professionals and patients, medical equipment, water, paper, laundry, construction (facilities, maintenance), sanitary structure, waste management (hospital Incineration; home waste landfill), vascular access surgery, and outpatient visits to determine the carbon footprint of dialysis patients9.
The total carbon footprints were:
- For Haemodialysis in a hospital: 3818 kg of CO2 Eq per patient, per year.
- For standard home haemodialysis: 4346 kg CO2 Eq per patient, per year.
- For Home Haemodialysis with NxStage system: 1844 kg of CO2 Eq per patient, per year.
The study concluded that most of the emissions are generated in medical equipment 37%, energy 21% and transport of patients 20%.
The low rate with NxStage system is due to several points where CO2 emissions, can be saved such as: transportation of nurses and the patient, water, laundry, construction of facilities, sanitary structure and outpatient visits to the hospital.
It is proven that increasing the frequency of dialysis will improve clinical outcomes (see chapter 3). However increased HD frequency is directly related to an increase of CO2 emissions into the atmosphere.
The carbon footprint of dialysis is influenced more by the frequency of treatments than by their duration.
The incorporation of emerging technologies, such as NxStage equipment, into HD programs might offer a possible solution to this problem. It is also clear that the carbon footprints of other new technologies should be evaluated.
11.2 Water
11.2.1 Water purification process
A patient who is on dialysis three times a week for four hours, has direct blood contact with 360 liters of water. With regard to water consumption, it should be also considered that a water treatment may run continuously even when dialysis machines are idle and production capacity is commonly oversized to ensure higher flows during disinfection of dialysis machines. If this water is not treated and purified morbidity and mortality would be high. Unfortunately water treatment spends a lot of energy to transform drinking water into water meeting international standards for dialysis. There are several general recommendations on how water treatment should reach the quality of ultrapure water once it has been treated: a double stage of osmosis, or a stage with a second element composed of one or a combination of the following: A) UV lamp plus ultrafilter; B) ultrafilter; C) electrode ionizer4. European norms describe how to build, certify and maintain the performance of a water treatment for HD as well as the quality required for HD fluids in “Guidance for the preparation and quality management of fluids for haemodialysis and related therapies”, ISO 23500:2014 and in “Quality of dialysis fluid for haemodialysis and related therapies”, ISO 11663:2014.
Nevertheless these norms do not consider the green aspect of dialysis fluids production. The ratio of water needed to produce dialysate water in a RO system can be 10:1 (i.e. for each liter of water produced by the RO system, 10 liters of water are required, of which 9 liters are discarded through the drain as waste-water). This entails a significant need for water supply, with the corresponding high cost for water.
The NxStage machine only requires about 30 liters of pure water for each session. Obviously the amount of water required is dependent on session prescription. NxStage either uses dialysate bags ready to use, or can prepare a batch of dialysate with PureFlowSL. It prepares up to 60 liters of ultra-pure dialysate which is fully utilized. With a modern deionisation technology, incoming water is converted into ultrapure product water on a 1:1 basis, so that one liter of product water is prepared with one liter of tap water. The PureFlow SL system prepares batches of 40, 50 or 60 liters of dialysate which, according to the patient’s prescription, can be used in up to three treatments.
PureFlow SL minimizes the workload related to the supply, conservation, management and disposal of prepackaged bags of dialysate fluid. Each bag of concentrate (SAK) replaces eight to twelve bags of five liters of premixed dialysate, depending on the patient’s prescription9.
The value of water consumed for one week in PureFlow SL treatments is, on average, the cost of doing laundry in a normal top-loading washing machine.
Infrastructure wise PureFlow SL requires simple installation compared to standard HD machines. PureFlow SL only requires a simple connection to the water outlet, so it is not necessary to make plumbing modifications to install the system in the home. The connection of the water is made through a simple adapter to the tap, to the socket of the washing machine or to the socket under the sink.
PureFlow SL works with standard domestic electricity. It uses a standard power cord, so it is not necessary for an electrician to install the PureFlow SL system8.
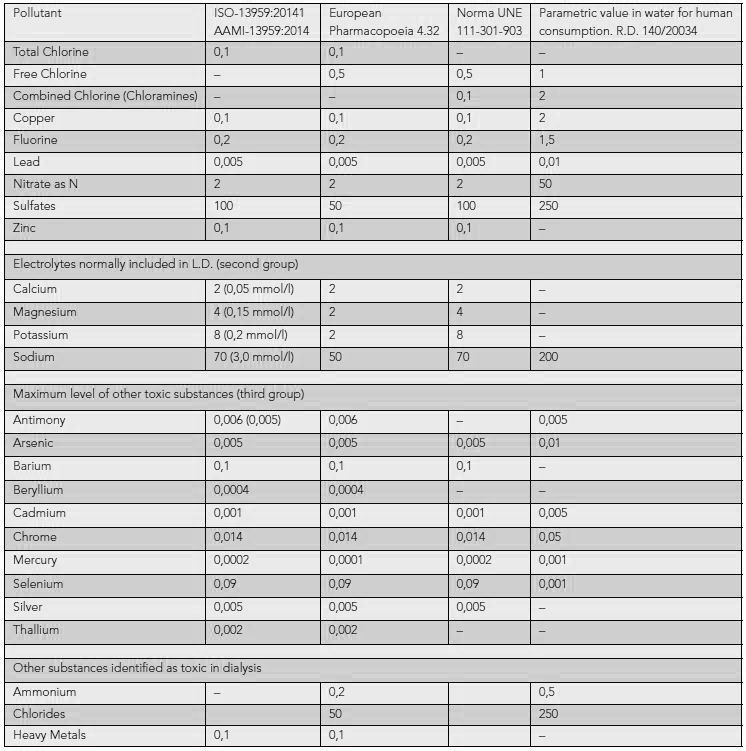
11.2.2 Standards for water purification
Europe has standard measures for water quality and design-validation of a water treatment4 (Appendix 1). For further details, please read “Guidance for the preparation and quality management of fluids for haemodialysis and related therapies”, ISO 23500:2014 and “Quality of dialysis fluid for haemodialysis and related therapies”, ISO 11663:2014.
Design of a water treatment plant for haemodialysis: includes different stages that can be defined as: 1. Preparation, 2. Pre-treatment, 3. Treatment and 4. Distribution.
- The preparation of water consists of removing most of the particles in suspension. This step is usually achieved by filters eliminating particles by sedimentation. To achieve a higher performance, filters in series will be placed, from higher to lower porosity.
- Pre-treatment should achieve the highest possible elimination of particles, the disappearance of chloramines and other organic matter and the decrease of the amount of cations. This process uses filters such as activated carbon.
- Treatment: The fundamental element in most water treatments is reverse osmosis (RO), and currently the quality standard is to have two stages of osmosis in series.
- Distribution of treated water is propelled by a pressure pump, through the distribution circuit, to the haemodialysis machines5.
11.2.3 Strategies for recycling water
Other ways to reduce water usage in haemodialysis include recycling of waste RO water (not relevant to the NxStage machine) or the use of waste RO for other functions such as garden watering or washing.
11.3 Electricity
11.3.1 Electricity consumption
In-centre treatment of patients with haemodialysis leaves a large environmental footprint, using high levels of power (approximately 1,000 kilowatt per hours (kWh) which is partly used creating the 80,000 L of water per patient, per year). RO water is energy-expensive to produce6.
Approximately 2.5 – 3.5 kWh are used for standard haemodialysis machines. In addition to electricity used for treatment of water, heating and air conditioning. Transporting, extracting and consuming this energy all contribute to the carbon footprint9.
Approximately 0.1kWh are used by the NxStage machine during dialysis10.
11.3.2 Strategies to reduce electricity consumption
The objective is to reduce energy expenditure with measures such as;
- Low energy lighting.
- Structure and orientation of the building reducing heating or airconditioning needs.
- Decreased volume of water treatment.
- Minimal run-time of machines and any other equipment – use of standby.
Lighting:
Modern LEDs are more energy efficient. This promising technology can save more than 50% (in some situations it can reach 90% compared to traditional technologies) when compared to standard lighting and provide the added advantage of superior lamp life.
Use of motion sensors, daylight sensors, timers and varied options to regulate the level of illumination may also reduce energy use.
Also it may be possible to modulate the level of illumination so that it is adjusted to the requirements of the activities that are being carried out. One example is that the lights in a dialysis room are dim and only increase when medical activities are in demand. Individual modulation: concentrate the lighting only in areas and times when it is necessary.
Heating and cooling:
The requirements of professionals and patients frequently do not match. Patients are often very sensitive to cold air in treatment areas. Normally they sit or lie passively during the treatment so they do not generate energy or body temperature, also dialysis is an exothermic therapy but extracorporeal circulation is cooling down blood temperature. Patients are especially sensitive to cold air currents. The staff is usually moving most of the time, so they cope with slightly cooler air1.
- Temperature: Ideally set an indoor temperature of 19 to 21°C in winter and 22 to 26°C in summer.
- Orientation of the building: the main façade would have to be facing south and avoid the windows facing west, so as to take advantage of the light and heat of the sun.
- Thermal insulation can reduce the need for heating and cooling considerably.
- Windows: double glazing saves 25% of energy in heating and isolates from outside noise.
- Blinds: help to ventilate the house in summer and block the sun. They retain heat in the winter.
- Adjusting dialysate temperatures (balance with risks of hypotension) and provision of blankets may reduce the need for excessive heating for patients.
Dialysate production:
The PureFlow SL maximum electrical usage is 400W per hour, but usage occurs intermittently when the dialyser heating plates in the PureFlow SL case hub are on. The average electric charge of the PureFlow SL when used at room temperature (18 to 22°C) is equivalent to a single light beam of 100W in continuous operation. This adds up to approximately 70 kilowatt hours (kWh) per month.
The installation and use of the PureFlow SL system does not significantly alter the environment and comfort of the patient’s home9.
Additional ways to save energy:
If possible we should use medical devices that are efficient for energy saving. All devices must be identified if they can be switched to “stand-by” or “off” after a treatment, at night or on weekends.
11.4 Logistics
11.4.1 The key carbon producing logistics
The logistics involve several factors that are indispensable to the operation of each HD unit. These can be:
- Laundry
- Catering
- Production of consumables such as plastics
- Energy
- Transport (patient and staff)
- Transport (consumables – internal and external)
Connor et al. compared the carbon footprint according to a study for transport3.
| In-centre - kgCO2Eq | NxStage - kgCO2Eq | |
| Patient | 747 | 19 |
| Staff | 175 | 28 |
11.4.2 Strategies to improve logistic efficiency
Reducing transport of both people and consumables affords the greatest opportunity for reducing energy expenditure. Car-pooling, public transport, transferring patients to dialysis units close to home and of course increased uptake of home dialysis all reduce transport usage.
Simple strategies are often the best. Encourage reuse of blankets, energy efficient cooking methods, recycling of plastics and obtaining supplies from a closer source.
11.5 Waste
11.5.1 Defining waste
Waste is any substance which is discarded after primary use, or it is worthless, defective and of no use. Examples include municipal solid waste (household trash/refuse), hazardous waste, waste water (including sewage and surface run-off) and radioactive waste.
- HHD NxStage equipment dialysis treatments produce waste of 179 kg CO2 Eq3.
- HHD standard equipment produces 208 kg CO2 Eq3.
11.5.2 Waste disposal
There are many waste disposal systems:
- Municipal waste includes household waste, commercial waste, and demolition waste.
- Hazardous waste includes industrial waste.
- Biomedical waste includes clinical waste.
- Special hazardous waste includes radioactive waste, explosive waste, and electronic waste (e-waste).
- Recycling of many substances including reusable plastics and paper.
Biomedical waste is any kind of waste containing infectious (or potentially infectious) materials and requires a specific disposal network. Incineration expends high energy levels to reach high temperatures that eliminate all pollutants and harmful to public health.
Domestic waste, which does not constitute a danger to public health can be disposed in a routine disposal process or recycled.
11.5.3 Strategies to reduce waste disposal carbon footprint
It is important to minimise waste going to incineration and maximise disposing of any non-contaminated waste into general waste or recycling. The use of two bins, one for contaminated and one for non-contaminated waste can reduce incineration needs. Also needles have to be disposed in an appropriate secured container.
Assess if the non-contaminated waste can be recycled. Teach patients and check if waste is being disposed correctly.
Both hospitals and community offer recycling and it is important to take advantage of any local recycling opportunities. Recycling is becoming more important and there are many new plastic and crystal materials that can be recycled7. Dialysis units can select products that are recyclable; such as bags, some housing, cardboard packaging, plastic wrapping, plastic caps. Taking advantage to separate in dedicated containers, as we do when sorting domestic waste, to recycle.
11.6 Implementing environmental change
To protect our environment it is important to review every step that constitutes logistics, power and water utilisation.
- Appoint an environmental officer to the dialysis unit who considers strategies for both in center and HHD.
- Educate all staff.
- Make environment part of the training program for patients.
- Choose a simple strategy to improve the environment for dialysis patients in your unit.
- Before choosing hardware for your patients, check utilities characteristics: power (kWh), water saving features, disinfection cycles.
- Prefer cleaning and disinfection procedures that limit use of chemicals.
Appendix 1. Water standards
Summary
Everyone is responsible for the environment. Everyone can contribute to reduce the increasing carbon footprint, each effort is valuable.
It is possible nowadays to measure pollution in Kg CO2 Eq7.
Nurses and patients must be educated so that they can make correct choices about how to reduce the carbon footprint because dialysis care has a serious impact with huge volumes of water, high power and disinfection chemicals usage.
Climate change remains a worldwide concern for governments, businesses and citizens. More information is currently being issued on the emissions produced by certain types of activities, events or even the day-to-day life of a person on foot; and the calculation of the carbon footprint can help us to answer all these questions.
Learning Activity
- If the patient chooses to perform haemodialysis at home, it will be important to assume the responsibility, normally carried out by the staff of the centre?
- What strategies do we know to reduce electricity consumption?
- What factors can increase the carbon footprint in a dialysis centre?
- What is the best option for haemodialysis technique, to reduce the carbon footprint?
- What amount of drinking water do we need to transform into pure water in a dialysis centre? And at home, with a deionisation system?
EDTNA/ERCA Secretariat
E-mail: secretariat@edtnaerca.org







